Appendicitis
Content of This Page
1- Introduction
2- Causes
3- Pathophysiology
4- Signs & Symptoms
5- Differential Diagnosis
6- Risk Factors
7- Investigations & Lab Results
8- Complications
9- Treatment
Introduction
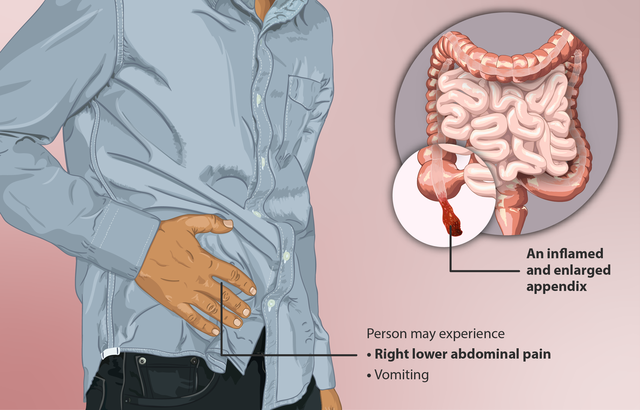
Appendicitis is an acute inflammation of the vermiform appendix, a narrow, finger-like pouch attached to the cecum in the right lower quadrant of the abdomen. It is one of the most common causes of acute abdominal pain requiring emergency surgery, especially in young adults. The condition occurs when the lumen of the appendix becomes obstructed, leading to increased pressure, inflammation, ischemia, and possible infection. If left untreated, appendicitis can progress to serious complications such as perforation, abscess formation, or peritonitis. Prompt diagnosis and surgical removal of the appendix (appendectomy) are the mainstays of treatment to prevent complications and reduce morbidity.
Causes
Lumen obstruction (most common overall cause)
Fecalith (hardened stool)
Lymphoid hyperplasia (common in children and young adults)
Parasitic infections (e.g., Enterobius vermicularis)
Foreign bodies (rare)
Tumors (e.g., carcinoid tumor, adenocarcinoma)
Strictures or fibrosis of the appendiceal lumen
Trauma (rare trigger)
Pathophysiology
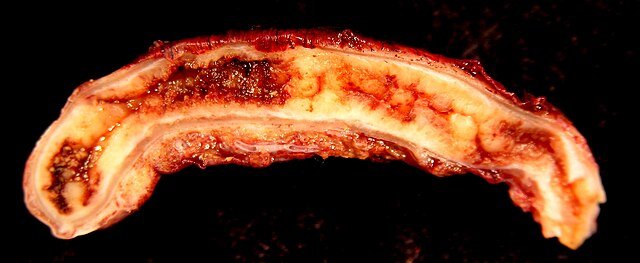
Appendicitis begins with obstruction of the appendiceal lumen, commonly due to fecalith, lymphoid hyperplasia, or other causes. This obstruction leads to accumulation of mucus and secretions, causing increased intraluminal pressure. The rising pressure impairs venous outflow, resulting in mucosal ischemia and weakening of the appendiceal wall. Ischemia promotes bacterial overgrowth, leading to inflammation, suppuration, and edema of the appendix. If the process continues, it can progress to necrosis and eventual perforation, spilling infectious contents into the peritoneal cavity and causing peritonitis or localized abscess formation
Sign & Symptoms
Abdominal pain
Starts as periumbilical pain
Shifts to the right lower quadrant (RLQ) (McBurney’s point)
Nausea and vomiting
Anorexia (loss of appetite)
Low-grade fever
Constipation or diarrhea (less common)
Rebound tenderness in RLQ
Guarding and abdominal rigidity (signs of peritonitis)
Rovsing’s sign – RLQ pain when pressing on the LLQ
Psoas sign – pain on hip extension (retrocecal appendix)
Obturator sign – pain with internal rotation of flexed right hip (pelvic appendix)
Elevated pulse and sometimes mild tachycardia
Differential Diagnosis
Gastroenteritis
Mesenteric adenitis
Meckel’s diverticulitis
Right-sided ureteric colic
Urinary tract infection (UTI)
Ectopic pregnancy
Ovarian torsion
Ruptured ovarian cyst
Pelvic inflammatory disease (PID)
Crohn’s disease (terminal ileitis)
Intestinal obstruction
Testicular torsion (referred pain in males)
Diverticulitis (right-sided, especially in elderly)
Risk Factors
Age: Most common in children and young adults (10–30 years)
Male sex: Slightly higher incidence in males
Diet: Low fiber, high refined carbohydrate intake
Family history: Genetic predisposition
Infections: Viral or bacterial infections causing lymphoid hyperplasia
Previous abdominal infections or inflammation
Obstruction: Presence of fecalith or foreign bodies in appendix

Investigations & Lab Results
Complete Blood Count (CBC):
Leukocytosis (increased white blood cells)
Neutrophilia (raised neutrophil count)
C-reactive Protein (CRP):
Elevated, indicating inflammation
Urinalysis:
To exclude urinary tract infection or hematuria
Pregnancy Test (β-hCG):
To exclude ectopic pregnancy in females of childbearing age
Imaging:
Abdominal Ultrasound:
Enlarged, non-compressible appendix (>6 mm diameter)
Free fluid or abscess
Useful especially in children and pregnant women
CT Scan Abdomen and Pelvis:
More sensitive and specific
Shows enlarged appendix, periappendiceal fat stranding, abscess, or perforation
MRI:
Alternative in pregnancy or when radiation is a concern
Complications
Perforation leading to peritonitis
Appendiceal abscess formation
Sepsis and systemic infection
Wound infection (post-appendectomy)
Intestinal obstruction (due to adhesions)
Appendiceal rupture causing generalized peritonitis
Fistula formation (rare)
Treatment
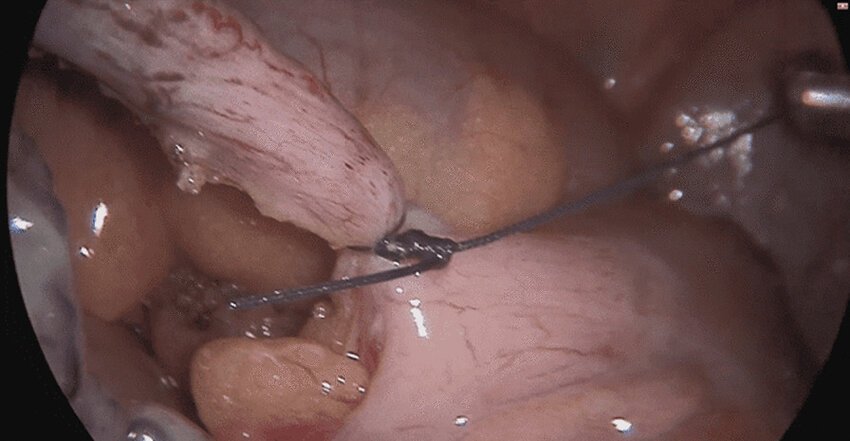
Surgical Removal (Appendectomy)
Laparoscopic appendectomy (preferred)
Open appendectomy (if laparoscopic not available or complicated cases)
Antibiotic Therapy
Preoperative broad-spectrum antibiotics
Postoperative antibiotics if perforation or abscess present
Conservative Management
Selected cases with uncomplicated appendicitis may be managed with antibiotics alone (controversial)
Supportive Care
IV fluids
Pain management
NPO (nothing by mouth) until surgery
Drainage
Percutaneous drainage for appendiceal abscess in stable patients before surgery