Caput Medusae
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
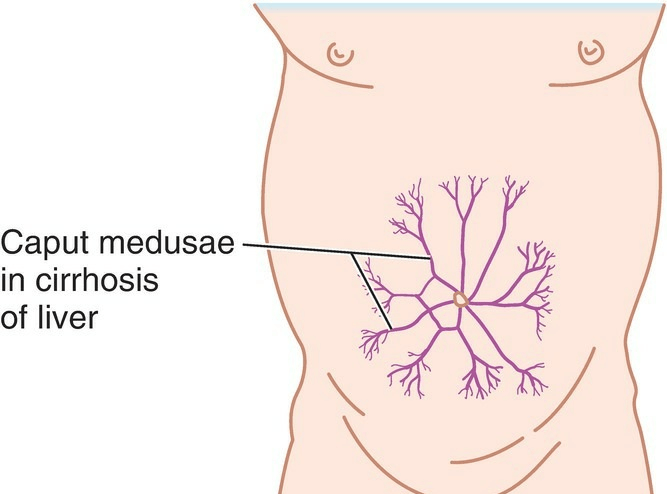
Caput medusae, which translates to “head of Medusa” in Latin, is a term used to describe a specific physical manifestation of portal hypertension, a condition characterized by increased pressure within the portal vein system. This phenomenon is named after the mythological creature Medusa, whose head was adorned with snakes.
Anatomical Overview
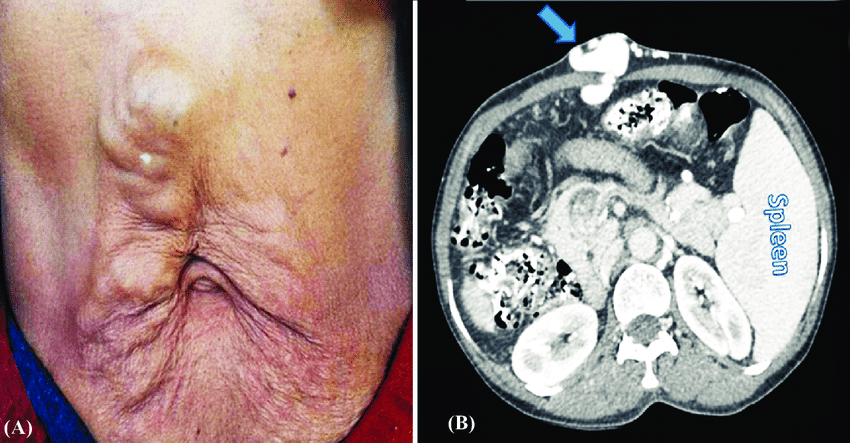
When scarring and fibrosis from cirrhosis obstruct the hepatic portal vein in the liver, pressure rises in the vein and its tributaries, producing portal hypertension. The large volume of blood flowing from the portal system to the systemic system at the sites of portal–systemic anastomoses may produce varicose veins, especially in the lower esophagus. The veins may become so dilated that their walls rupture, resulting in hemorrhage. Bleeding from esophageal varices (abnormally dilated veins) at the distal end of the esophagus is often severe and may be fatal. In severe cases of portal obstruction, the veins of the anterior abdominal wall (normally caval tributaries) that anastomose with the para-umbilical veins (normally portal tributaries) may become varicose and look somewhat like small snakes radiating under the skin around the umbilicus. This condition is referred to as caput medusae because of its resemblance to the serpents on the head of Medusa, a character in Greek mythology.
Causes
Liver Cirrhosis: This is the most common cause of portal hypertension and caput medusae. Cirrhosis is a late stage of scarring (fibrosis) of the liver caused by many forms of liver diseases and conditions, such as chronic alcoholism, viral hepatitis, and nonalcoholic fatty liver disease.
Portal Vein Thrombosis: Blood clots in the portal vein can obstruct blood flow, leading to increased pressure within the portal vein system and the development of collateral circulation, including caput medusae.
Budd-Chiari Syndrome: This rare condition involves the obstruction or narrowing of the veins that carry blood from the liver (hepatic veins). When blood flow out of the liver is compromised, it can lead to portal hypertension and the development of caput medusae.
Constrictive Pericarditis: In some cases, conditions affecting the heart, such as constrictive pericarditis, can cause increased pressure in the portal vein system, leading to the development of collateral circulation and caput medusae.
Hepatic Veno-Occlusive Disease (VOD): VOD is a condition characterized by obstruction of the small veins in the liver. This obstruction can lead to portal hypertension and the development of caput medusae.
Schistosomiasis: In regions where this parasitic infection is prevalent, chronic infection with Schistosoma parasites can lead to liver fibrosis, portal hypertension, and caput medusae.
Treatment
Management of Underlying Liver Disease: If caput medusae is caused by liver cirrhosis or other liver diseases, treatment focuses on managing the underlying condition. This may include lifestyle modifications (such as abstinence from alcohol for alcoholic liver disease), medications to manage symptoms and complications, and, in some cases, liver transplantation for end-stage liver disease.
Portal Hypertension Management: Controlling portal hypertension is essential in managing caput medusae. This may involve medications to reduce portal vein pressure, such as beta-blockers like propranolol or nadolol. Other medications, like non-selective beta-blockers and vasopressin analogs, may also be used to reduce portal pressure.
Variceal Bleeding Prevention: Caput medusae is often associated with the development of varices, which are enlarged, fragile veins in the esophagus or stomach. Variceal bleeding is a severe complication of portal hypertension. Preventive measures to reduce the risk of variceal bleeding may include endoscopic procedures such as band ligation or sclerotherapy to treat varices and prevent bleeding.
Shunt Procedures: In some cases of severe portal hypertension, surgical or radiological procedures may be performed to create a shunt (a connection) between the portal vein and another vein to redirect blood flow and reduce pressure in the portal vein system. These procedures include transjugular intrahepatic portosystemic shunt (TIPS) and surgical portosystemic shunts.
Liver Transplantation: For individuals with end-stage liver disease and severe portal hypertension, liver transplantation may be considered. This involves replacing the diseased liver with a healthy liver from a deceased or living donor. Liver transplantation can effectively resolve portal hypertension and its complications, including caput medusae.
Symptomatic Management: Symptomatic relief measures may also be employed to alleviate discomfort associated with caput medusae, such as wearing compression garments to reduce venous pooling and discomfort.