Femoral Hernia
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
A femoral hernia is a type of hernia that occurs in the groin area where the abdominal contents, typically part of the intestine or abdominal fat, protrude through a weakened area or hole in the abdominal wall. Unlike inguinal hernias, which are more common, femoral hernias occur lower down and are less frequent but can pose significant health risks if not treated promptly.

Anatomical Overview
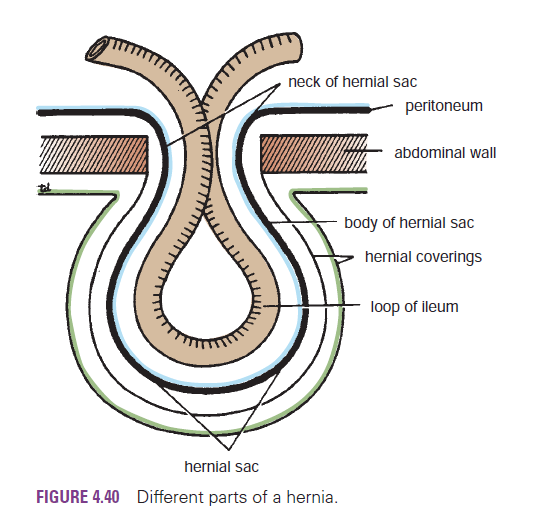
The femoral ring is a weak area in the anterior abdominal wall that normally is of a size sufficient to admit the tip of the little finger. The femoral ring is the usual originating site of a femoral hernia, a protrusion of abdominal viscera (often a loop of small intestine) through the femoral ring into the femoral canal. A femoral hernia appears as a mass, often tender, in the femoral triangle, inferolateral to the pubic tubercle.The hernia is bounded by the femoral vein laterally and the lacunar ligament medially. The hernial sac compresses the contents of the femoral canal (loose connective tissue, fat, and lymphatics) and distends the wall of the canal. Initially, the hernia is small because it is contained within the canal, but it can enlarge by passing inferiorly through the saphenous opening into the subcutaneous tissue of the thigh. Femoral hernias are more common in females because of their wider pelves and smaller inguinal canals and rings. This type of hernia may also occur after multiple pregnancies due to enlargement of the femoral ring over time from increased intra-abdominal pressure forcing fat into the femoral canal. Femoral hernias may cause hip or abdominal pain. Strangulation of a femoral hernia may occur because of the sharp, rigid boundaries of the femoral ring, particularly the concave margin of the lacunar ligament. Strangulation of a femoral hernia interferes with the blood supply to the herniated intestine. This vascular impairment may result in necrosis (death of the tissues).
Causes
Increased Intra-Abdominal Pressure: Activities or conditions that increase pressure within the abdomen can contribute to the formation of a hernia. These include:
- Heavy lifting
- Chronic coughing
- Straining during bowel movements or urination
- Obesity
- Pregnancy
- Ascites (accumulation of fluid in the abdomen)
Muscle Weakness: Weakness in the muscles of the abdominal wall or groin can make it easier for tissue to push through. Factors contributing to muscle weakness include:
- Aging
- Previous surgery in the groin or abdominal area
- Genetic predisposition to weaker connective tissues
Injury or Strain: Trauma or injury to the groin area can weaken the muscles and increase the risk of a hernia.
Gender: Women are more likely to develop femoral hernias than men, possibly due to the wider bone structure of the female pelvis.
History of Hernias: Having a personal or family history of hernias increases the likelihood of developing a femoral hernia.
Treatment
1. Surgical Repair
There are two primary types of surgery used to repair a femoral hernia:
a. Open Surgery
- Procedure: The surgeon makes an incision near the site of the hernia to access the herniated tissue. The tissue is pushed back into place, and the weakened area is reinforced with sutures, mesh, or both.
- Recovery: Recovery time can vary but typically involves several weeks of restricted activity to allow the repair to heal properly.
b. Laparoscopic Surgery
- Procedure: This minimally invasive surgery involves several small incisions through which the surgeon inserts a laparoscope (a thin tube with a camera) and surgical instruments. The hernia is repaired using similar techniques as in open surgery, often involving the placement of mesh to strengthen the area.
- Recovery: Recovery from laparoscopic surgery is usually quicker than from open surgery, with patients often returning to normal activities within a few days to a week.
2. Non-Surgical Management
While surgery is the definitive treatment for femoral hernias, certain patients may be managed non-surgically in specific circumstances, such as those who are at high risk for surgery due to other medical conditions. Non-surgical management includes:
- Observation: Monitoring the hernia for any signs of complications such as pain, changes in size, or signs of strangulation.
- Lifestyle Modifications: Advising the patient to avoid heavy lifting and manage factors that increase intra-abdominal pressure, such as chronic coughing or constipation.