Polycystic Ovary Syndrome
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It is characterized by the presence of multiple small cysts on the ovaries, irregular menstrual cycles, and elevated levels of androgens (male hormones).
The exact cause of PCOS is unknown, but it is believed to involve a combination of genetic and environmental factors. Insulin resistance, obesity, and inflammation are also thought to play a role.
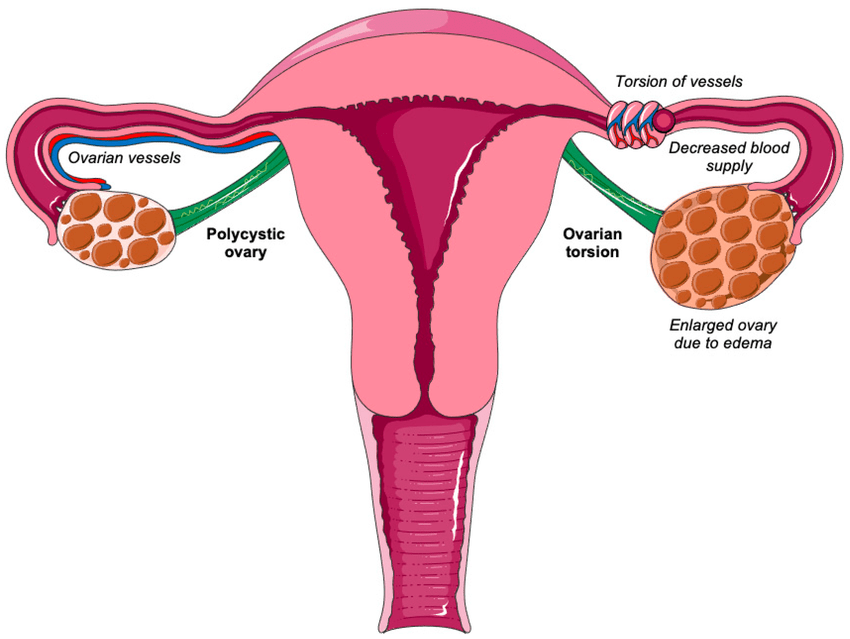
Anatomical Overview
Polycystic Ovary Syndrome (PCOS) primarily affects the ovaries, which are the female reproductive organs responsible for producing eggs and hormones such as estrogen and progesterone. In PCOS, the ovaries contain numerous small, fluid-filled sacs called follicles or cysts, each typically less than 8mm in size. These cysts are immature follicles that have not developed properly due to hormonal imbalances, particularly elevated levels of androgens (male hormones). The hormonal imbalance also disrupts the regular ovulation process, leading to irregular or absent menstrual cycles.
In addition to the ovaries, PCOS can impact other parts of the body. The endocrine system, which includes the pituitary gland, adrenal glands, and pancreas, is often involved due to insulin resistance commonly seen in PCOS patients. Insulin resistance can lead to higher insulin levels, which further exacerbate androgen production. The excess androgens affect various tissues, contributing to symptoms like hirsutism (excess hair growth), acne, and alopecia (hair loss). The metabolic disturbances associated with PCOS also increase the risk of developing obesity, type 2 diabetes, and cardiovascular diseases.

Causes
Genetic Predisposition: PCOS tends to run in families, suggesting a genetic component. Women with a family history of PCOS are more likely to develop the condition. Multiple genes are thought to be involved, affecting various aspects of hormone production and insulin regulation.
Insulin Resistance: Insulin resistance is a significant factor in PCOS. It occurs when the body’s cells do not respond effectively to insulin, leading to higher levels of insulin in the bloodstream. Elevated insulin levels can increase androgen production by the ovaries, contributing to symptoms like hirsutism and acne. Insulin resistance is also associated with weight gain, which can further exacerbate PCOS symptoms.
Hormonal Imbalances: Women with PCOS often have elevated levels of androgens (male hormones) such as testosterone. This hormonal imbalance can interfere with the normal development and release of eggs during the menstrual cycle, leading to irregular or absent ovulation. The exact mechanism behind increased androgen production in PCOS is not fully understood but is linked to insulin resistance and other factors.
Low-Grade Inflammation: Many women with PCOS have low-grade inflammation, which can stimulate the ovaries to produce androgens. Inflammation is also associated with insulin resistance and obesity, creating a complex interplay of factors that contribute to PCOS.
Excessive Luteinizing Hormone (LH): Elevated levels of LH, produced by the pituitary gland, can stimulate the ovaries to produce more androgens. This imbalance between LH and follicle-stimulating hormone (FSH) can disrupt normal ovarian function.
Lifestyle Factors: Diet, physical activity, and body weight can influence the development and severity of PCOS. Obesity, in particular, is strongly associated with insulin resistance and hormonal imbalances. However, PCOS can also occur in women of normal weight.
Treatment
- Diet and Exercise: A healthy diet and regular physical activity are crucial in managing PCOS. Weight loss can improve insulin resistance, lower androgen levels, and regulate menstrual cycles. Even a modest reduction in weight (5-10%) can have significant benefits.
- Stress Management: Reducing stress through practices like yoga, meditation, and counseling can help manage symptoms and improve overall well-being.
Medications:
- Hormonal Contraceptives: Birth control pills, patches, or vaginal rings containing estrogen and progestin can help regulate menstrual cycles, reduce androgen levels, and improve acne and hirsutism.
- Anti-Androgens: Medications such as spironolactone can block the effects of androgens and reduce symptoms like excessive hair growth and acne.
- Metformin: Often used to treat type 2 diabetes, metformin can improve insulin resistance and lower insulin levels, helping to regulate menstrual cycles and reduce androgen levels in women with PCOS.
- Fertility Treatments: For women trying to conceive, medications like clomiphene citrate or letrozole can stimulate ovulation. In more complex cases, assisted reproductive technologies like in vitro fertilization (IVF) may be considered.
Surgical Options:
- Ovarian Drilling: A minimally invasive surgical procedure called laparoscopic ovarian drilling can reduce androgen production and stimulate ovulation in women who do not respond to medication.
Cosmetic Treatments:
- For symptoms like hirsutism and acne, treatments may include topical creams, laser hair removal, and dermatological procedures.
Mental Health Support:
- Addressing mental health is important, as PCOS is often associated with depression and anxiety. Counseling, support groups, and therapy can be beneficial.