Benign Prostatic Hyperplasia (BPH)
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
Benign Prostatic Hyperplasia (BPH), also known as prostate gland enlargement, is a common condition that affects aging men. The prostate gland, a walnut-sized gland located just below the bladder, surrounds the urethra, the tube that carries urine from the bladder out of the body.
Anatomical Overview
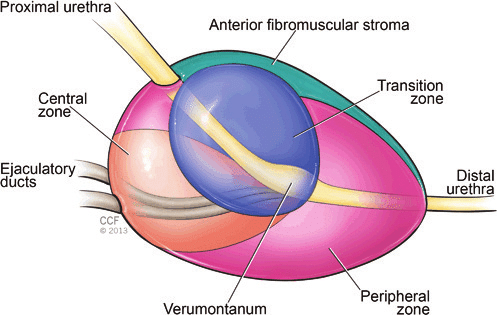
Benign Prostatic Hyperplasia (BPH) involves the non-cancerous enlargement of the prostate gland, a small walnut-sized gland that is part of the male reproductive system. To understand BPH, let’s delve into the anatomical details of the prostate gland and its surrounding structures:
Location: The prostate gland is located just below the bladder and surrounds the urethra, which is the tube that carries urine from the bladder out through the penis. Its position gives the prostate gland a significant role in urinary function.
Anatomy: The prostate gland consists of several lobes or regions. It is divided into anterior, posterior, lateral, and median lobes. The urethra passes through the prostate gland, and its location in the gland affects the urinary flow.
Function: The primary function of the prostate gland is to produce and secrete seminal fluid, a milky substance that nourishes and transports sperm during ejaculation. The prostate gland’s secretions contribute to the composition of semen.
Histology: The prostate gland is composed of glandular tissue and smooth muscle. The glandular tissue contains specialized cells called glandular epithelial cells, which produce prostate-specific antigen (PSA) and other substances found in prostatic fluid.
Vascularization and Innervation: The prostate gland receives its blood supply from branches of the internal iliac arteries. It is richly innervated by both sympathetic and parasympathetic nerve fibers, which play a role in controlling urinary and sexual function.
Age-related Changes: As men age, the prostate gland may undergo changes known as benign prostatic hyperplasia (BPH). In BPH, the glandular tissue of the prostate proliferates, leading to an increase in the size of the gland. This enlargement can cause compression of the urethra, leading to urinary symptoms.

Causes
Hormonal Changes: Hormonal changes associated with aging are considered a primary factor in the development of BPH. Testosterone, the primary male sex hormone, is converted to dihydrotestosterone (DHT) by an enzyme called 5-alpha reductase. DHT is believed to stimulate the growth of prostate cells. As men age, the balance of hormones in the body shifts, leading to an increase in DHT levels and possibly contributing to prostate enlargement.
Age: BPH is primarily a condition of aging. The prevalence of BPH increases with age, with most men experiencing some degree of prostate enlargement by their 60s and 70s. However, not all men will develop symptomatic BPH.
Genetics: There is evidence to suggest that genetics may play a role in predisposing individuals to BPH. Men with a family history of BPH are more likely to develop the condition themselves.
Inflammation: Chronic inflammation within the prostate gland may contribute to the development of BPH. Inflammatory processes can lead to tissue damage and cellular proliferation, potentially contributing to prostate enlargement.
Lifestyle Factors: Certain lifestyle factors, such as obesity, lack of physical activity, and poor diet, may increase the risk of BPH. These factors are also associated with other conditions, such as metabolic syndrome, which may indirectly influence prostate health.
Other Medical Conditions: Certain medical conditions, such as diabetes and cardiovascular disease, have been associated with an increased risk of BPH. Additionally, medications used to treat these conditions, such as diuretics and anticholinergics, may exacerbate urinary symptoms associated with BPH.
Treatment
Watchful Waiting: For men with mild symptoms that do not significantly impact their quality of life, a “watchful waiting” approach may be recommended. This involves regular monitoring of symptoms without immediate intervention. Lifestyle modifications, such as limiting fluid intake before bedtime and avoiding caffeine and alcohol, may be suggested.
Medications:
- Alpha-Blockers: These medications relax the muscles of the prostate and bladder neck, improving urinary flow and relieving symptoms such as hesitancy, urgency, and weak stream.
- 5-Alpha Reductase Inhibitors: These medications work by blocking the conversion of testosterone to dihydrotestosterone (DHT), reducing the size of the prostate gland over time and relieving symptoms.
- Combination Therapy: Some men may benefit from a combination of alpha-blockers and 5-alpha reductase inhibitors, particularly those with larger prostates or severe symptoms.
- Other Medications: Other medications, such as phosphodiesterase-5 inhibitors or anticholinergics, may be prescribed to alleviate specific symptoms or complications associated with BPH.
Minimally Invasive Procedures:
- Transurethral Microwave Thermotherapy (TUMT): This procedure uses microwave energy to heat and destroy prostate tissue, relieving urinary obstruction.
- Transurethral Needle Ablation (TUNA): TUNA involves the insertion of needles into the prostate gland, which deliver radiofrequency energy to destroy excess tissue.
- Prostatic Urethral Lift (PUL): PUL is a minimally invasive procedure that involves the placement of small implants to lift and hold the enlarged prostate tissue away from the urethra, improving urinary flow.
- Water Vapor Thermal Therapy (Rezūm): This procedure uses steam to deliver thermal energy to the prostate tissue, causing cell death and shrinkage of the gland.
Surgery:
- Transurethral Resection of the Prostate (TURP): TURP is a traditional surgical procedure that involves the removal of excess prostate tissue using a resectoscope inserted through the urethra.
- Holmium Laser Enucleation of the Prostate (HoLEP): HoLEP utilizes laser energy to remove obstructive prostate tissue, offering a minimally invasive alternative to TURP.
- Open Prostatectomy: In rare cases of very large prostates, open surgery may be necessary to remove excess tissue.