Peptic ulcer
Content of This Page
1- Introduction
2- Causes
3- Pathophysiology
4- Signs & Symptoms
5- Types of Peptic Ulcer
6- Risk Factors
7- Investigations & Lab Results
8- Complications
9- Treatment
Introduction
Peptic Ulcer is a break or sore in the mucosal lining of the stomach (gastric ulcer) or the duodenum (duodenal ulcer), caused by an imbalance between aggressive factors like gastric acid and pepsin and defensive mechanisms such as the mucus-bicarbonate barrier, prostaglandins, and adequate blood flow. The most common cause is infection with Helicobacter pylori, a bacterium that damages the mucosal lining and promotes inflammation. Another major cause is the chronic use of nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit prostaglandin synthesis, reducing mucosal protection. Other contributing factors include smoking, alcohol, stress, and genetic predisposition.

Causes
Helicobacter pylori infection
NSAIDs (Nonsteroidal Anti-Inflammatory Drugs)
Stress (severe illness, burns, trauma)
Zollinger-Ellison syndrome (gastrinoma)
Smoking
Alcohol consumption
Excessive caffeine intake
Genetic predisposition
Hypersecretory states
Malignancy (gastric cancer can mimic ulcers)
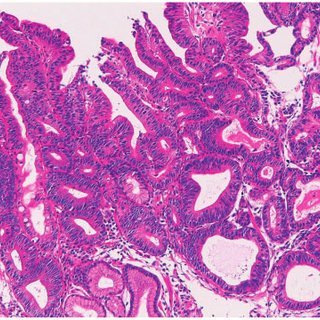
Pathophysiology
Peptic Ulcer results from an imbalance between aggressive factors and the protective mechanisms of the gastric or duodenal mucosa. Increased aggressive factors such as gastric acid and pepsin cause mucosal damage. Helicobacter pylori infection contributes by damaging the mucosa and increasing acid secretion. NSAIDs impair mucosal defenses by inhibiting prostaglandin synthesis, which reduces mucus and bicarbonate production. Smoking and alcohol further decrease mucosal blood flow and impair healing. At the same time, a reduction in protective factors like mucus secretion, bicarbonate, mucosal blood flow, epithelial regeneration, and prostaglandins leads to weakened mucosal defense. This imbalance ultimately results in mucosal injury and ulcer formation. In Zollinger-Ellison syndrome, excessive acid secretion caused by a gastrin-secreting tumor leads to multiple and difficult-to-treat ulcers.
Signs & Symptoms
Epigastric pain (burning or gnawing)
Pain related to meals:
Duodenal ulcer: pain relieved by eating, recurs 2–3 hours after meals
Gastric ulcer: pain worsens with eating
Dyspepsia (indigestion)
Nausea and vomiting
Bloating and early satiety
Weight loss (especially in gastric ulcers)
Hematemesis or melena (if bleeding occurs)
Signs of perforation (acute severe abdominal pain, rigidity)
Anemia symptoms (fatigue, pallor) if chronic bleeding
Types of Peptic Ulcer
| Feature | Gastric Ulcer | Duodenal Ulcer |
|---|---|---|
| Location | Stomach (usually antrum) | First part of duodenum |
| Pain relation to food | Worsens with eating | Relieved by eating |
| Age group | Older adults | Younger adults |
| Acid secretion | Normal or decreased | Increased |
| Malignancy risk | Higher risk (needs biopsy) | Rarely malignant |
| Weight changes | Weight loss | normal |
| NSAIDs association | Strong association | Less association |
| Common cause | H. pylori, NSAIDs | H. pylori |
| Bleeding risk | Moderate | Higher risk |
Risk Factors
Helicobacter pylori infection
Regular or prolonged use of NSAIDs (aspirin, ibuprofen, etc.)
Smoking tobacco
Excessive alcohol consumption
High stress levels (especially severe physical stress like trauma or surgery)
Older age (mucosal defenses weaken with age)
Family history of peptic ulcers
Certain medical conditions (e.g., Zollinger-Ellison syndrome)
Use of corticosteroids or anticoagulants (which can increase bleeding risk)
Poor diet or irregular eating habits (less directly, but may worsen symptoms)
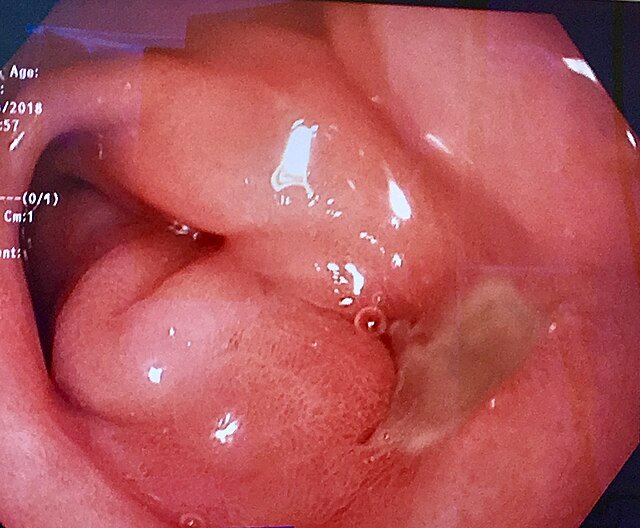
Investigations & Lab Results
-Endoscopy (Gold Standard)
Direct visualization of ulcer
Location, size, depth assessment
Biopsy to rule out malignancy (especially in gastric ulcers)
Rapid urease test for H. pylori detection
-H. pylori Testing
Urea breath test (non-invasive, highly sensitive)
Stool antigen test (non-invasive, reliable)
Serology for H. pylori antibodies (less preferred, can’t differentiate past vs. current infection)
Biopsy with histology (via endoscopy)
-Blood Tests
Complete blood count (CBC) – may show anemia if bleeding
Iron studies – may show iron deficiency anemia
Liver and renal function tests – to rule out other causes or pre-endoscopy check
Serum gastrin levels – elevated in Zollinger-Ellison syndrome
-Imaging (if perforation or obstruction suspected)
Abdominal X-ray – free air under diaphragm (perforation)
CT scan of abdomen – complications like perforation, penetration, or obstruction
Barium meal X-ray (less commonly used now) – shows ulcer crater or deformity
-Stool Occult Blood Test
Detects gastrointestinal bleeding (positive if ulcer is bleeding)
Complications
Bleeding (most common complication; can cause hematemesis or melena)
Perforation (sudden severe abdominal pain, peritonitis)
Penetration (ulcer extends into adjacent organs like pancreas)
Gastric outlet obstruction (due to edema or scarring)
Malignancy (especially in gastric ulcers)
Intractable pain
Fistula formation (rare)
Treatment
Eradication of H. pylori
Triple therapy: PPI + Clarithromycin + Amoxicillin/Metronidazole
Quadruple therapy (if resistance or failure): PPI + Bismuth + Metronidazole + Tetracycline
Acid Suppression
Proton Pump Inhibitors (PPIs) – mainstay (e.g., omeprazole, pantoprazole)
H2 receptor blockers – alternative (e.g., ranitidine, famotidine)
Stop NSAIDs
Discontinue NSAIDs if possible
Use PPIs if NSAIDs are necessary
Lifestyle Modifications
Smoking cessation
Avoid alcohol
Avoid caffeine and spicy foods
Stress management
Treatment of Complications
Bleeding: endoscopic hemostasis, PPI infusion, surgery if uncontrolled
Perforation: emergency surgery
Obstruction: endoscopic dilation or surgery
Penetration: manage surgically if severe
Surgery (rarely needed today)
For refractory ulcers, complications, or suspected malignancy