Tracheostomy
content of this page
1- Introduction
2- Anatomical Overview
3- Procedure
4- Clinical Significance
Introduction
Tracheostomy is a surgical procedure that involves creating a direct opening (stoma) into the trachea through the front of the neck. This procedure is performed to establish a secure airway for patients who require prolonged mechanical ventilation, have upper airway obstruction, or cannot maintain a clear airway due to various medical conditions.
Anatomical Overview
Anatomy of the Trachea and Neck:
Trachea (Windpipe):
- The trachea is a tubular structure extending from the larynx (voice box) to the main bronchi, where it bifurcates into the left and right bronchi leading to the lungs.
- It consists of rings of cartilage that provide structural support and prevent collapse.
Larynx (Voice Box):
- Situated above the trachea, the larynx houses the vocal cords and facilitates speech production.
- It is connected to the trachea via the cricoid cartilage, which forms a ring-like structure.
Thyroid Gland:
- Located in the front of the neck, the thyroid gland wraps around the trachea and plays a role in hormone production and metabolism.
Cricoid Cartilage and Cricothyroid Membrane:
- The cricoid cartilage is the only complete ring of cartilage around the trachea, located just below the thyroid cartilage.
- The cricothyroid membrane is a soft tissue structure between the cricoid and thyroid cartilages, easily palpable in the midline of the neck.
Vascular and Nervous Structures:
- Major blood vessels, such as the carotid arteries and jugular veins, run along the sides of the neck.
- Nerves, including the recurrent laryngeal nerve and vagus nerve, are important for vocal cord function and sensation in the larynx.
Procedure
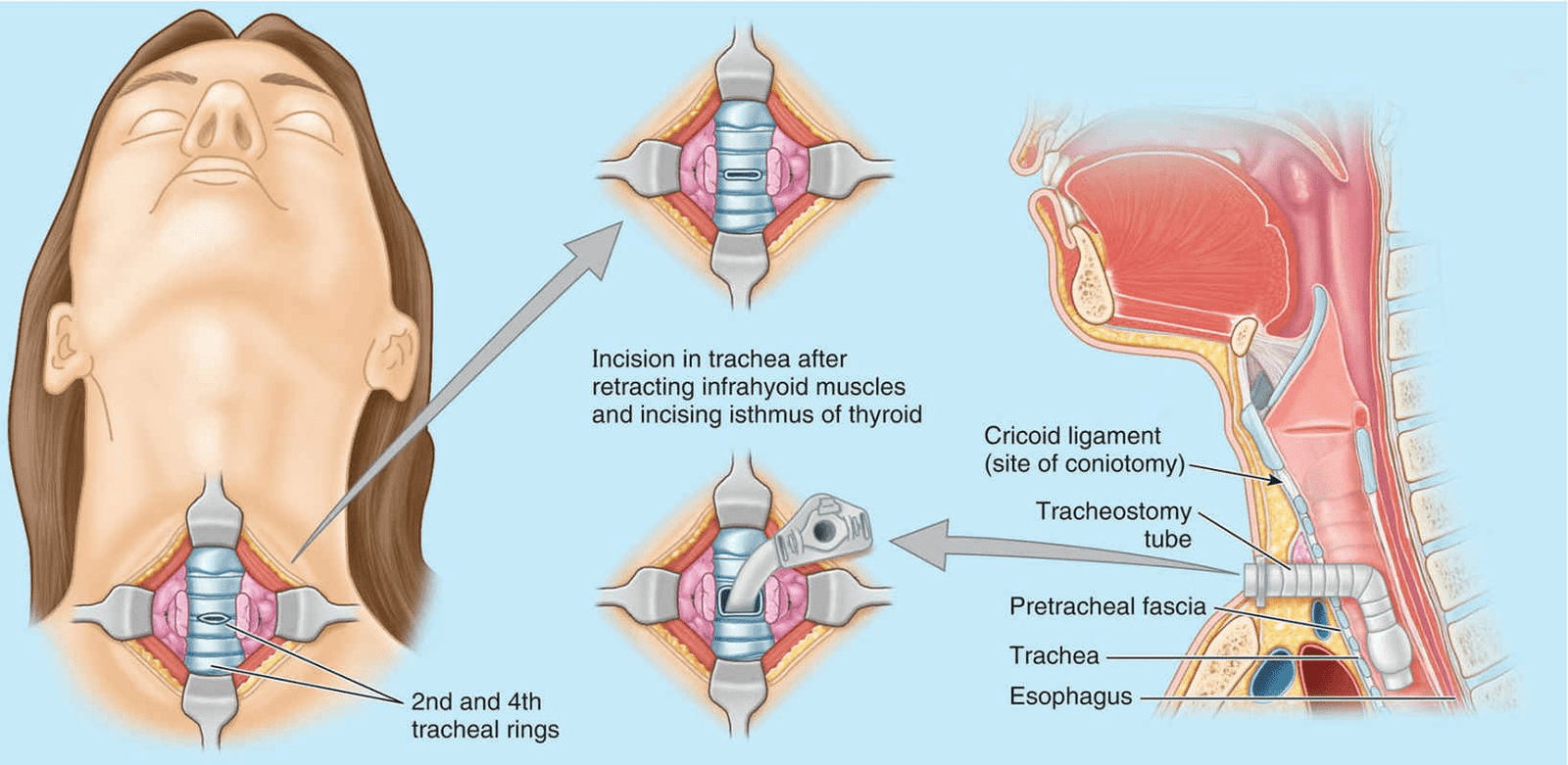
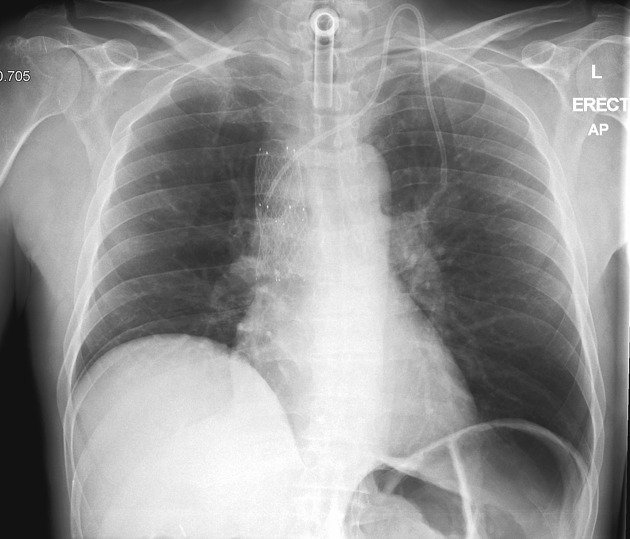
A transverse incision through the skin of the neck and anterior wall of the trachea, tracheostomy, establishes an airway in patients with upper airway obstruction or respiratory failure (Fig. B9.13). The infrahyoid muscles are retracted laterally, and the isthmus of the thyroid gland is either divided or retracted superiorly. An opening is made in the trachea between the first and second tracheal rings or through the second through fourth rings. A tracheostomy tube is then inserted into the trachea and secured. To avoid complications during a tracheostomy, the following anatomical relationships are important:
- The inferior thyroid veins arise from a venous plexus on the thyroid gland and descend anterior to the trachea.
- A small thyroid ima artery is present in approximately 10% of people; it ascends from the brachiocephalic trunk or the arch of the aorta to the isthmus of the thyroid gland.
- The left brachiocephalic vein, jugular venous arch, and pleurae may be encountered, particularly in infants and children.
- The thymus covers the inferior part of the trachea in infants and children.
- The trachea is small, mobile, and soft in infants, making it easy to cut through its posterior wall and damage the esophagus.
Clinical Significance
Respiratory Support and Ventilation: Tracheostomy allows for direct access to the trachea, enabling long-term mechanical ventilation in patients who require prolonged respiratory support. This is particularly beneficial for individuals with respiratory failure due to conditions such as chronic obstructive pulmonary disease (COPD), neuromuscular disorders, or severe pneumonia.
Airway Management in Critical Care: In critically ill patients who cannot maintain a clear airway, tracheostomy ensures continuous airflow and facilitates effective secretion management. It reduces the risk of upper airway obstruction and aspiration, which can be life-threatening in intensive care settings.
Facilitation of Weaning from Ventilation: Tracheostomy may aid in the weaning process from mechanical ventilation by reducing airway resistance and enabling easier trials of spontaneous breathing. This can lead to earlier liberation from ventilator support and potentially shorter hospital stays.
Improved Patient Comfort and Communication: Compared to endotracheal intubation, which can cause discomfort and hinder communication, tracheostomy tubes are better tolerated over the long term. Patients can speak more naturally, eat orally (if permitted), and maintain better oral hygiene, improving their overall quality of life during recovery.
Management of Upper Airway Obstruction: Tracheostomy is crucial in managing upper airway obstructions due to tumors, trauma, infections, or congenital anomalies. By bypassing the obstruction, it ensures continuous airflow to the lungs and prevents respiratory distress.
Long-term Care and Rehabilitation: Tracheostomy supports patients undergoing prolonged rehabilitation, allowing them to participate in physical therapy and regain strength without the limitations of endotracheal intubation.
Emergency Airway Access: In emergency situations where rapid access to the airway is essential, such as in cases of severe trauma or failed intubation attempts, tracheostomy can be lifesaving by providing a secure airway until further interventions can be performed.
Palliative Care and Comfort Measures: In palliative care settings, tracheostomy may be considered to alleviate respiratory distress and enhance comfort for patients with terminal illnesses.