Facial Nerve Palsy
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
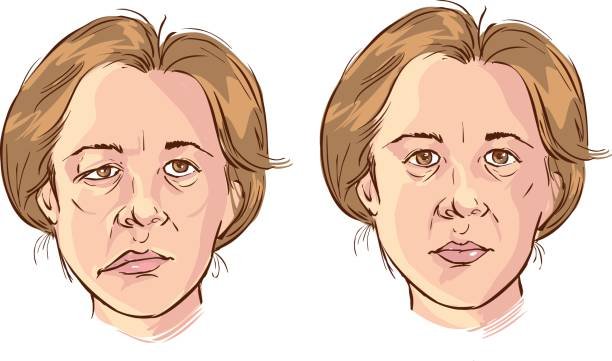
Facial nerve palsy, also known as facial paralysis, is a condition characterized by the inability to move facial muscles on one or both sides of the face. This paralysis occurs due to damage or dysfunction of the facial nerve, which controls the muscles of facial expression, as well as other important functions such as taste sensation from the anterior two-thirds of the tongue and tear production.
Anatomical Overview
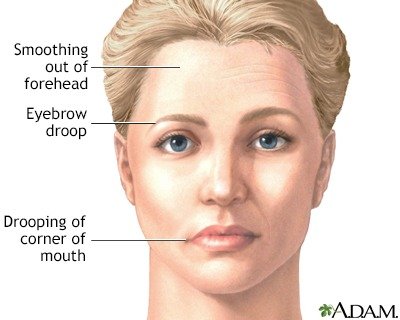
Injury to branches of the facial nerve causes paralysis of the facial muscles (Bell palsy), with or without loss of taste on the anterior two thirds of the tongue or altered secretion of the lacrimal and salivary glands. Lesions near the origin of CN VII from the pons of the brain, or proximal to the origin of the greater petrosal nerve (in the region of the geniculate ganglion), result in loss of motor, gustatory (taste), and autonomic functions. Lesions distal to the geniculate ganglion, but proximal to the origin of the chorda tympani nerve, produce the same dysfunction, except that lacrimal secretion is not affected. Lesions near the stylomastoid foramen result in loss of motor function only (i.e., facial paralysis). Facial nerve palsy has many causes. The most common nontraumatic cause of facial paralysis is inflammation of the facial nerve near the stylomastoid foramen, often as a result of a viral infection. This produces edema (swelling) and compression of the nerve in the facial canal. Injury of the facial nerve may result from fracture of the temporal bone. Facial paralysis is evident soon after the injury. If the nerve is completely sectioned, the chances of complete or even partial recovery are remote. Muscular movement usually improves when the nerve damage is associated with blunt head trauma; however, recovery may not be complete (Russo et al., 2016). Facial nerve palsy may be idiopathic (occurring without a known cause). However, it often follows exposure to cold, as occurs when riding in a car with a window open. Facial paralysis may be a complication of surgery; consequently, identification of the facial nerve and its branches is essential during surgery (e.g., parotidectomy, removal of a parotid gland). The facial nerve is most distinct as it emerges from the stylomastoid foramen. If necessary, electrical stimulation may be used for confirmation. Facial nerve palsy may also be associated with dental manipulation, vaccination, pregnancy, HIV infection, Lyme disease (inflammatory disorder causing headache and stiff neck), and infections of the middle ear (otitis media).
Causes
Bell’s Palsy: Bell’s palsy is the most common cause of acute facial nerve paralysis. It is believed to be due to inflammation of the facial nerve (cranial nerve VII), often triggered by viral infections, particularly herpes simplex virus (HSV).
Idiopathic Causes: In many cases, no specific cause can be identified for facial nerve palsy, especially when it occurs suddenly (acute). This is termed idiopathic facial nerve palsy.
Trauma: Injury to the head, skull fractures, or facial trauma can damage the facial nerve, leading to paralysis. Surgical procedures involving the head or face can also inadvertently injure the facial nerve.
Infections:
- Viral Infections: Besides HSV (associated with Bell’s palsy), other viruses such as herpes zoster (shingles), Epstein-Barr virus (EBV), and influenza viruses can cause facial nerve inflammation and paralysis.
- Bacterial Infections: Lyme disease, caused by Borrelia burgdorferi bacteria transmitted by ticks, is known to cause facial nerve palsy, often accompanied by other neurological symptoms.
- Otitis Media: Middle ear infections can spread to involve the facial nerve, resulting in facial paralysis.
Neoplastic Causes: Tumors affecting the skull base or the parotid gland (e.g., acoustic neuroma, parotid gland tumors) can compress or invade the facial nerve, leading to paralysis.
Autoimmune Disorders: Conditions like Guillain-Barré syndrome, sarcoidosis, or multiple sclerosis can cause immune-mediated inflammation of the facial nerve, resulting in paralysis.
Congenital Causes: Rarely, facial nerve palsy can be present at birth (congenital facial nerve palsy), often due to developmental abnormalities or birth trauma.
Neurological Disorders: Conditions affecting the central nervous system (CNS), such as stroke or brain tumors, can disrupt nerve signals and lead to facial nerve palsy.
Metabolic Causes: Conditions like diabetes mellitus or hypothyroidism can affect nerve function and increase susceptibility to nerve damage, including the facial nerve.
Iatrogenic Causes: Damage to the facial nerve can occur as a complication of surgical procedures involving the head, neck, or ear region.
Treatment
Medical Management:
Corticosteroids: Corticosteroid medications, such as prednisone, are commonly prescribed early in cases of Bell’s palsy or idiopathic facial nerve palsy to reduce inflammation around the facial nerve and promote faster recovery. Steroids may also be used in other types of facial nerve palsy to reduce swelling and inflammation.
Antiviral Medications: If the facial nerve palsy is associated with a viral infection, such as herpes simplex virus (HSV), antiviral medications may be prescribed in addition to steroids to target the underlying viral cause.
Eye Care: Protecting the eye on the affected side is crucial to prevent complications like corneal ulceration due to reduced or absent blinking. This may involve the use of lubricating eye drops, eye patches at night, or taping the eye shut during sleep.
2. Physical Therapy:
Facial Exercises: Specific exercises and techniques prescribed by a physical therapist or facial rehabilitation specialist can help strengthen facial muscles, improve muscle tone, and restore facial symmetry. These exercises may include smiling, frowning, raising eyebrows, and puckering lips.
Massage and Manual Therapy: Gentle massage techniques and manual manipulation of facial muscles can help improve circulation, reduce muscle stiffness, and promote healing.
3. Surgical and Procedural Interventions:
Botulinum Toxin Injections (Botox): Botulinum toxin injections can be used to temporarily weaken or paralyze overactive muscles on the unaffected side of the face, which can help improve facial symmetry and reduce involuntary movements (synkinesis) during recovery.
Surgical Procedures: In cases where facial nerve damage is severe or irreversible, surgical interventions may be considered:
- Facial Nerve Decompression: This procedure involves removing bone or tissue around the facial nerve to relieve pressure and allow for nerve healing.
- Facial Nerve Repair: Surgical repair or grafting of the facial nerve may be performed in cases of nerve injury or trauma.
- Facial Reanimation Surgery: Techniques such as nerve transfers, muscle transfers, or placement of facial slings may be used to restore facial movement and symmetry.
4. Supportive and Symptomatic Care:
Eye Protection: Ensuring adequate eye protection with artificial tears, moisture chamber glasses, or eye patches is essential to prevent complications related to reduced eye closure and tear production.
Emotional and Psychological Support: Coping with facial nerve palsy can be emotionally challenging due to changes in appearance and facial expression. Counseling or support groups may be beneficial to address psychological effects and improve overall well-being.
5. Management of Underlying Conditions:
- Treatment of Underlying Causes: If facial nerve palsy is secondary to conditions such as infections, tumors, or autoimmune disorders, appropriate treatment of the underlying condition is essential for improving facial nerve function.