Horner's Syndrome
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
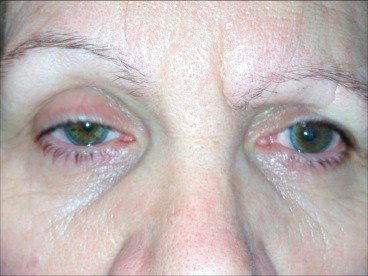
Horner’s syndrome is a rare condition that affects the nervous system, specifically the nerves that control the muscles of the face and eye. It is characterized by a combination of symptoms that can include drooping of the upper eyelid (ptosis), constriction of the pupil (miosis), sinking of the eyeball into the eye socket (enophthalmos), and lack of sweating (anhidrosis) on one side of the face.

Anatomical Overview
Trauma: Injuries to the head, neck, or chest can damage the sympathetic nerves.
Tumors: Both benign and malignant tumors can compress or infiltrate the sympathetic nerves. Tumors can be located in the chest, neck, or brain.
Stroke: A stroke affecting the brainstem or the pathway of the sympathetic nerves can lead to Horner’s syndrome.
Infections: Infections such as tuberculosis, syphilis, or Lyme disease can affect the sympathetic nerves.
Surgery: Procedures in the neck, chest, or brain can inadvertently damage the sympathetic nerves.
Cluster Headaches: These severe headaches can sometimes be associated with Horner’s syndrome.
Other Neurological Conditions: Conditions such as multiple sclerosis or syringomyelia can lead to Horner’s syndrome.
Idiopathic: In some cases, no underlying cause can be identified, and the syndrome is classified as idiopathic.
Causes
Stroke: A stroke can lead to agnosia if it disrupts blood flow to the areas of the brain involved in sensory processing, particularly the occipital, parietal, or temporal lobes. This deprivation of oxygen and nutrients can cause neurons to die, leading to impaired sensory recognition.
Traumatic Brain Injury (TBI): Severe head injuries can damage brain regions associated with sensory perception and integration. The impact can cause direct damage to the brain tissue or secondary complications such as bleeding, swelling, and pressure that further injure these areas.
Neurodegenerative Diseases: Conditions such as Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease can progressively damage the brain over time, including areas involved in sensory processing. As these diseases advance, they can lead to various forms of agnosia.
Brain Tumors: Tumors in the brain can press on or invade regions involved in sensory processing, leading to agnosia. Both benign and malignant tumors can cause such disruptions depending on their location and size.
Infections: Brain infections like encephalitis or meningitis can cause inflammation and damage to the brain tissue, potentially affecting areas involved in sensory recognition. This damage can result from the infection itself or from the body’s immune response to the infection.
Anoxia/Hypoxia: Conditions that lead to insufficient oxygen supply to the brain, such as cardiac arrest, respiratory failure, or severe anemia, can cause widespread brain damage. If the sensory processing regions are affected, agnosia can result.
Neurological Disorders: Other disorders like multiple sclerosis or epilepsy can sometimes cause agnosia if they affect the relevant brain areas. Multiple sclerosis, for example, can cause demyelination in pathways involved in sensory processing.
Surgical Complications: Rarely, complications from brain surgery can lead to damage in sensory processing areas, resulting in agnosia.
Treatment
Observation: If Horner’s syndrome is mild and not causing significant symptoms, a wait-and-watch approach may be recommended.
Underlying Condition Treatment: Treating the condition causing Horner’s syndrome, such as surgery for tumors or antibiotics for infections.
Medications:
- Apraclonidine eye drops: These drops can help improve ptosis (drooping eyelid) and miosis (constricted pupil) by stimulating the dilator muscle of the iris.
- Phenylephrine eye drops: These drops can also be used to dilate the pupil on the affected side.
- Artificial tears: To manage dryness and discomfort in the eye due to reduced tear production.
Surgery: In some cases, surgery may be necessary to correct underlying structural issues or to relieve compression on the sympathetic nerves.
Physical Therapy: Exercises to improve eye muscle strength and coordination may be beneficial, especially if ptosis is affecting vision.
Eye Protection: In cases of decreased tear production, it’s important to protect the eye from irritation and injury.
Counseling and Support: Coping with the symptoms of Horner’s syndrome can be challenging, and counseling or support groups may be helpful.