Pes Planus (Flat Feet)
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
Pes planus, commonly known as flat feet, is a condition where the arches of the feet are flattened, causing the entire sole of the foot to make contact with the ground when standing. This can occur in one or both feet and may be present from birth or develop over time. Flat feet can vary in severity, with some individuals experiencing no symptoms, while others may suffer from foot pain, stiffness, or problems with balance and posture.
Anatomical Overview
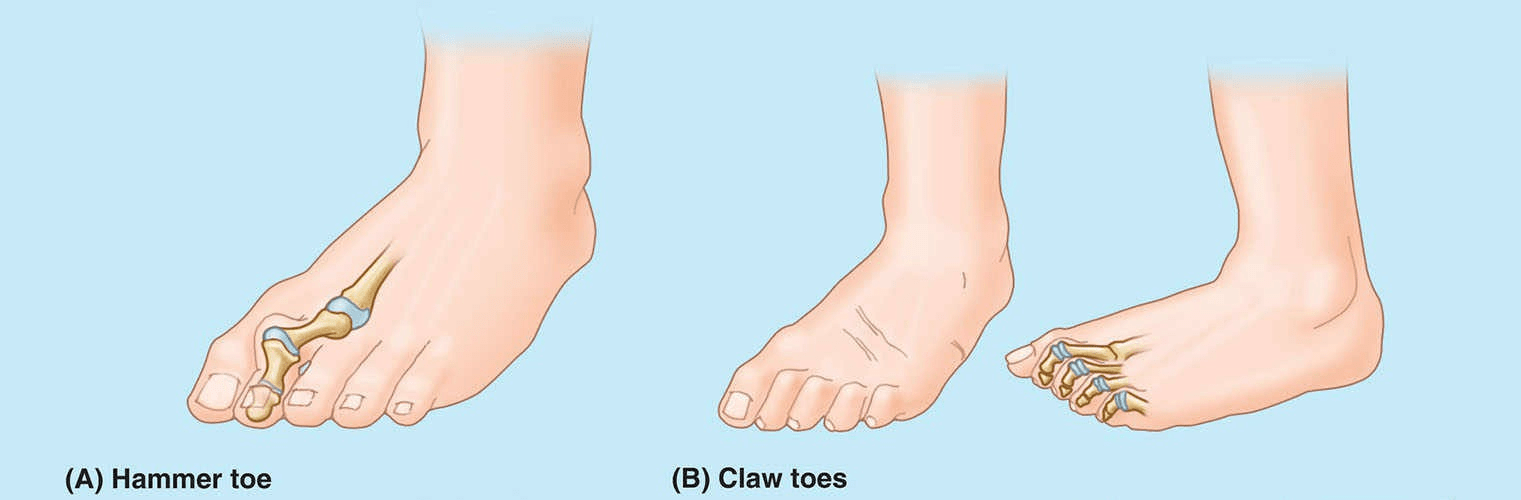
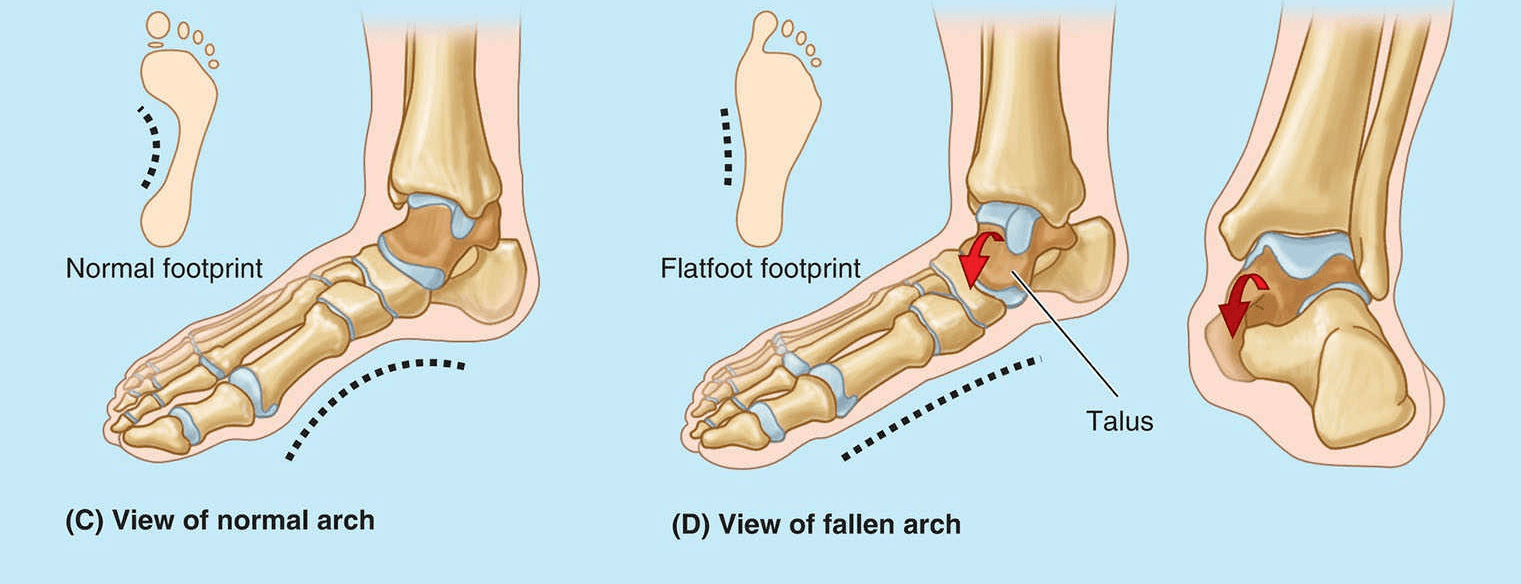
The flat appearance of the sole of the foot before age 3 is normal; it results from the thick subcutaneous fat pad in the sole. As children get older, the fat is lost, and a normal medial longitudinal arch becomes visible. Flat feet can either be flexible (flat, lacking a medial arch, when weight bearing but normal in appearance when not bearing weight or rigid (flat even when not bearing weight). The more common flexible flat feet result from loose or degenerated intrinsic ligaments (inadequate passive arch support). Flexible flat feet is common in childhood but usually resolves with age as the ligaments grow and mature. The condition occasionally persists into adulthood and may or may not be symptomatic.
Rigid flat feet with a history that goes back to childhood are likely to result from a bone deformity (such as a fusion of adjacent tarsal bones). Acquired flat feet (“fallen arches”) are likely to be secondary to dysfunction of the tibialis posterior (dynamic arch support) owing to trauma, degeneration with age, or denervation. In the absence of normal passive or dynamic support, the plantar calcaneonavicular ligament fails to support the head of the talus. Consequently, the head of the talus displaces inferomedially and becomes prominent, As a result, some flattening of the medial part of the longitudinal arch occurs, along with lateral deviation of the forefoot. Flat feet are common in older people, particularly if they undertake much unaccustomed standing or gain weight rapidly, adding stress on the muscles and increasing the strain on the ligaments supporting the arches.
Causes
Genetics: Family history plays a significant role in the development of flat feet. If one or both parents have flat feet, there’s a higher likelihood that their children will inherit the condition.
Weak Arches: Sometimes, the arches of the feet may not develop properly during childhood, leading to flat feet. Weakness in the muscles and tendons that support the arch can contribute to its collapse.
Foot Injuries: Trauma or injury to the foot, such as fractures or dislocations, can cause the arches to flatten over time.
Muscle or Nerve Diseases: Conditions such as muscular dystrophy, cerebral palsy, or nerve problems (e.g., neuropathy) can affect muscle strength and control in the feet, potentially leading to flat feet.
Rheumatoid Arthritis: Inflammatory diseases like rheumatoid arthritis can cause inflammation and damage to the joints and tissues of the feet, altering their structure and contributing to flat feet.
Aging: As we age, the tendons and ligaments in the feet may weaken or stretch, causing the arches to gradually fall.
Obesity: Excess weight can put additional stress on the feet and contribute to the development of flat feet.
Pregnancy: Hormonal changes during pregnancy can relax the ligaments in the body, including those in the feet, potentially leading to flat feet or exacerbating an existing condition.
Treatment
Orthotic Devices: Custom-made orthotic inserts or arch supports can help support the arch and distribute pressure more evenly across the foot. These devices can be worn inside shoes and are tailored to individual foot contours and needs.
Footwear Modifications: Wearing supportive and properly fitting shoes is crucial. Shoes with good arch support and a firm heel counter can help stabilize the foot and reduce discomfort.
Physical Therapy: Specific exercises can strengthen the muscles and tendons in the feet and ankles, improving stability and alignment. A physical therapist can develop a personalized exercise program based on individual needs.
Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen can help reduce pain and inflammation associated with flat feet, especially if there’s an inflammatory component.
Lifestyle Modifications: Maintaining a healthy weight and avoiding activities that exacerbate symptoms (such as prolonged standing or high-impact sports) can help manage discomfort.
Steroid Injections: In some cases, corticosteroid injections may be recommended to reduce inflammation and pain, particularly if there is inflammation of the tendons or joints in the feet.
Surgery: Surgical intervention is typically considered only for severe cases of flat feet that do not respond to conservative treatments. Surgical procedures can involve realigning bones, repairing tendons, or fusing joints to improve foot function and alleviate pain.