Chest Tube
content of this page
1- Introduction
2- Anatomical Overview
3- Procedure
4- Clinical Significance
Introduction
Anatomical Overview
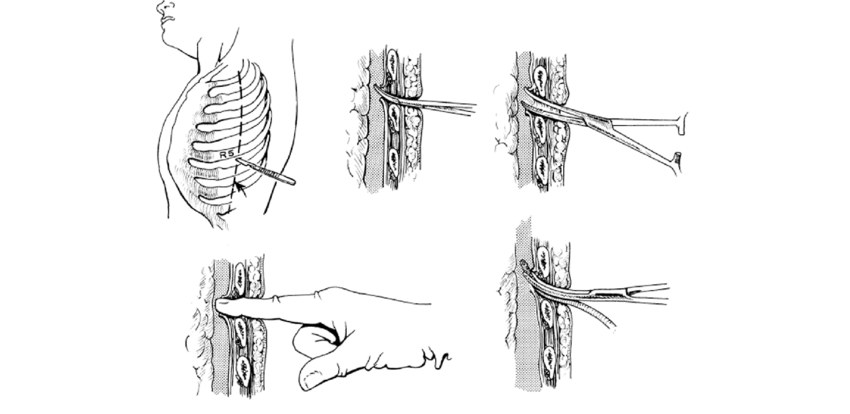
Major amounts of air, blood, serous fluid, pus, or any combination of these substances in the pleural cavity are typically removed by insertion of a chest tube. A short incision is made in the 5th or 6th intercostal space in the midaxillary line (which is approximately at nipple level). The tube may be directed superiorly (toward the cervical pleura for air removal or inferiorly (toward the costodiaphragmatic recess) for fluid drainage. The extracorporeal end of the tube (i.e., the end that is outside of the body) is connected to an underwater drainage system, often with controlled suction, to prevent air from being sucked back into the pleural cavity. Removal of air allows reinflation of a collapsed lung. Failure to remove fluid may cause the lung to develop a resistant fibrous covering that inhibits expansion unless it is peeled off (lung decortication).
Procedure
Preparation:
- Explain the procedure to the patient, addressing any concerns and obtaining informed consent.
- Position the patient comfortably, usually in a semi-recumbent or sitting position.
- Gather necessary equipment, including a chest tube kit, sterile drapes, local anesthetic, suture material, and a drainage system.
Sterile Preparation:
- Clean and sterilize the insertion site, typically the fourth or fifth intercostal space in the mid-axillary line on the affected side.
- Drape the area with sterile drapes, leaving the insertion site exposed.
Anesthesia:
- Administer local anesthesia to the skin and deeper tissues along the planned insertion site to minimize discomfort during the procedure.
Incision:
- Make a small incision (usually around 2-3 cm) at the selected insertion site using a scalpel or a sharp instrument.
Insertion:
- Insert the chest tube through the incision, directing it superiorly and posteriorly into the pleural space.
- Advance the tube until the desired length is reached, ensuring that the distal end of the tube lies within the pleural cavity.
Confirmation:
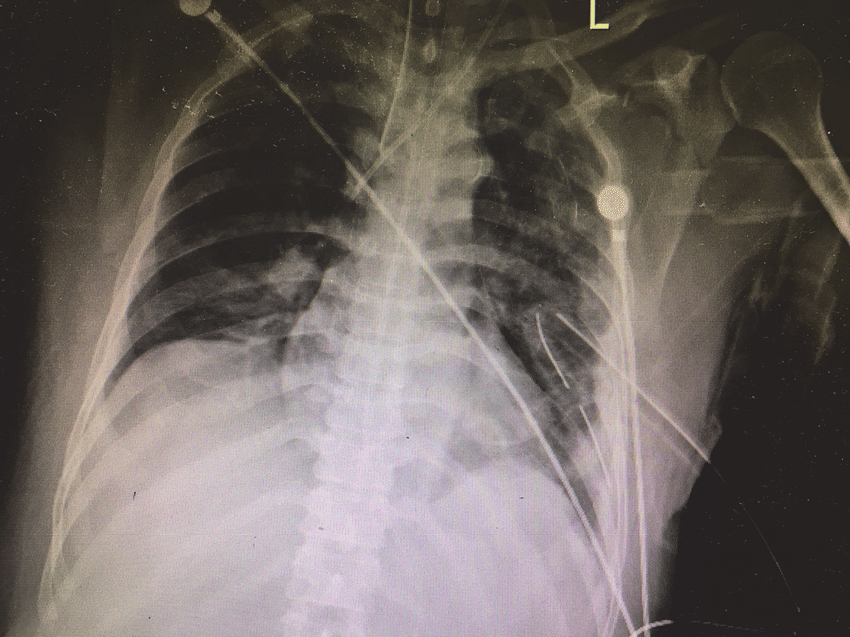
- Confirm the correct placement of the chest tube by observing air or fluid drainage into the collection system.
- Perform a chest X-ray to verify the position of the chest tube and assess lung re-expansion.
Securing the Tube:
- Secure the chest tube to the skin using sutures or adhesive dressing to prevent accidental dislodgement.
- Apply a sterile occlusive dressing around the insertion site to maintain a closed system.
Connection to Drainage System:
- Connect the proximal end of the chest tube to a sterile drainage system, ensuring that all connections are secure and airtight.
- Set the drainage system to the appropriate suction level or water seal as indicated by the clinical condition.
Post-procedure Care:
- Monitor the patient closely for any signs of complications, such as respiratory distress, bleeding, or infection.
- Provide appropriate pain management and respiratory support as needed.
- Educate the patient about chest tube care, including drainage system maintenance, activity restrictions, and signs of potential complications.
Follow-up:
- Schedule follow-up assessments to monitor the patient’s clinical progress, chest tube drainage, and lung re-expansion.
- Consider chest tube removal once the underlying condition has resolved, and there is minimal or no drainage from the chest tube.
Clinical Significance
Management of Pneumothorax: Chest tubes are crucial in treating pneumothorax, a condition characterized by the presence of air in the pleural space, which can cause lung collapse. The chest tube allows for the removal of trapped air, re-expanding the lung and preventing further respiratory compromise.
Treatment of Pleural Effusion: Pleural effusion, the accumulation of fluid in the pleural space, can lead to respiratory distress and compromise lung function. Chest tubes facilitate the drainage of pleural fluid, relieving symptoms and preventing complications such as infection or pleural adhesions.
Control of Hemothorax: Hemothorax, the accumulation of blood in the pleural cavity often resulting from trauma or injury, requires prompt intervention to prevent respiratory compromise and hypovolemic shock. Chest tubes allow for the evacuation of blood from the pleural space, stabilizing the patient and facilitating the management of associated injuries.
Postoperative Drainage: Following thoracic surgery, chest tubes are often used to drain air, fluid, or blood from the surgical site, promoting lung expansion, preventing complications such as pneumothorax or pleural effusion, and facilitating postoperative recovery.
Management of Empyema: Empyema, a collection of pus in the pleural space usually secondary to infection, requires drainage to resolve the infection and prevent systemic spread. Chest tubes facilitate the evacuation of purulent material, allowing for effective antimicrobial therapy and promoting resolution of the infection.
Diagnosis and Treatment of Traumatic Injuries: Chest tubes may be inserted as part of the management of traumatic thoracic injuries, such as penetrating wounds or blunt trauma. They help to stabilize the patient, control bleeding, and prevent tension pneumothorax or hemothorax, allowing for further evaluation and definitive treatment.
Monitoring and Management of Thoracic Procedures: Chest tubes are often used in conjunction with thoracic procedures such as lung biopsies, thoracoscopy, or pleurodesis. They facilitate drainage, monitor for post-procedural complications such as air leaks or bleeding, and promote optimal post-procedure recovery.
Relief of Symptomatic Dyspnea: In certain cases of severe dyspnea or respiratory distress due to conditions such as severe pneumonia or acute respiratory distress syndrome (ARDS), chest tubes may be used as a temporizing measure to relieve pressure on the lungs and improve respiratory function.