Diaphragmatic Paralysis
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
Diaphragmatic paralysis is a condition characterized by the partial or complete loss of function of one or both hemidiaphragms, the primary muscle involved in respiration. This paralysis can result from various underlying causes, leading to impaired breathing mechanics and respiratory compromise. Understanding diaphragmatic paralysis is essential for recognizing its clinical significance and guiding appropriate management strategies.
Anatomical Overview
The diaphragm is a dome-shaped muscle that separates the thoracic cavity from the abdominal cavity and plays a crucial role in respiration. An anatomical overview of diaphragmatic paralysis involves understanding the structure and function of the diaphragm, as well as the implications of its paralysis.
Anatomy of the Diaphragm:
Structure: The diaphragm is a large, thin, musculotendinous structure that forms the floor of the thoracic cavity. It consists of a central tendon, peripheral muscular portions, and several openings for the passage of structures such as the inferior vena cava, esophagus, and aorta.
Attachments: The diaphragm attaches to the lower ribs, sternum, and vertebral column. Its central tendon is aponeurotic and lacks bony attachments.
Nerve Supply: The primary nerve supply to the diaphragm is provided by the phrenic nerves, which arise from the cervical nerve roots C3-C5. These nerves innervate the diaphragm and play a crucial role in its contraction during respiration.
Implications of Diaphragmatic Paralysis:
Respiratory Compromise: Diaphragmatic paralysis leads to impaired lung ventilation and respiratory mechanics, resulting in symptoms such as dyspnea, orthopnea, and respiratory distress. The affected lung may exhibit atelectasis (collapse) due to inadequate inflation.
Paradoxical Breathing: In some cases of unilateral diaphragmatic paralysis, paradoxical breathing may occur, where the affected side moves inward during inspiration and outward during expiration, leading to inefficient ventilation.
Reduced Exercise Tolerance: Patients with diaphragmatic paralysis may experience reduced exercise tolerance and exertional dyspnea due to compromised respiratory function.
Risk of Complications: Chronic diaphragmatic paralysis can lead to complications such as respiratory infections, ventilatory failure, and respiratory muscle weakness.

Causes
Neurological Causes:
- Phrenic Nerve Injury: Damage to the phrenic nerves, which innervate the diaphragm, can result in diaphragmatic paralysis. This injury can occur due to trauma, surgical procedures, compression, or neurological disorders affecting the cervical spine or nerve roots (e.g., cervical spine injury, brachial plexus injury, neuropathies).
- Neurodegenerative Diseases: Conditions such as amyotrophic lateral sclerosis (ALS), Guillain-Barré syndrome, multiple sclerosis, or other motor neuron diseases can lead to dysfunction of the phrenic nerves or their central connections, resulting in diaphragmatic paralysis.
Traumatic Causes:
- Thoracic Trauma: Blunt or penetrating trauma to the chest or abdomen can injure the diaphragm or the phrenic nerves, leading to diaphragmatic paralysis. Traumatic injuries may result from motor vehicle accidents, falls, gunshot wounds, or surgical procedures in the thoracic or abdominal regions.
- Surgical Trauma: Surgical interventions involving the thoracic or cervical regions, such as cardiac surgery, thoracic surgery, neck dissections, or procedures involving the brachial plexus, may inadvertently damage the phrenic nerves or the diaphragm, resulting in paralysis.
Iatrogenic Causes:
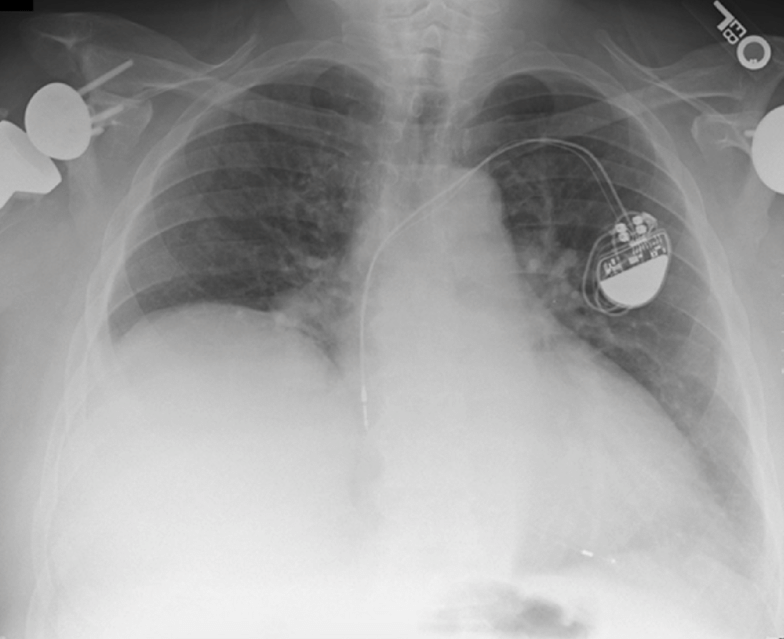
- Interventional Procedures: Certain medical procedures or interventions, such as central venous catheterization, pacemaker implantation, or radiofrequency ablation of cardiac arrhythmias, can lead to phrenic nerve injury or diaphragmatic paralysis as a complication.
- Mechanical Ventilation: Prolonged mechanical ventilation with high tidal volumes or excessive positive end-expiratory pressure (PEEP) can cause phrenic nerve injury or diaphragmatic dysfunction, leading to diaphragmatic paralysis or weakness (referred to as ventilator-induced diaphragmatic dysfunction).
Idiopathic Causes:
- In some cases, the exact cause of diaphragmatic paralysis may not be identified, and the condition is considered idiopathic. Idiopathic diaphragmatic paralysis may occur spontaneously or due to subtle underlying factors that are not readily apparent.
Miscellaneous Causes:
- Inflammatory or Infectious Conditions: Inflammatory processes affecting the diaphragm or surrounding structures, such as pleurisy, pneumonia, tuberculosis, or diaphragmatic myositis, can lead to diaphragmatic paralysis.
- Neoplastic Infiltration: Tumors or malignancies involving the phrenic nerves, cervical spine, or mediastinum may compress or infiltrate the nerves, leading to diaphragmatic paralysis.
Treatment
Respiratory Support:
- Non-Invasive Ventilation (NIV): NIV, such as continuous positive airway pressure (CPAP) or bilevel positive airway pressure (BiPAP), may be used to support respiratory function and alleviate symptoms of respiratory distress, especially in acute cases.
- Mechanical Ventilation: In severe cases of respiratory failure or compromised respiratory function, invasive mechanical ventilation may be necessary to provide ventilatory support and ensure adequate oxygenation.
Physical Therapy:
- Respiratory Muscle Training: Inspiratory and expiratory muscle training exercises, along with diaphragmatic breathing techniques, may help improve respiratory muscle strength and endurance.
- Postural Techniques: Certain postural maneuvers, such as leaning forward or sitting upright, may optimize lung mechanics and improve ventilation in patients with diaphragmatic paralysis.
Surgical Interventions:
- Diaphragmatic Plication: In cases of unilateral diaphragmatic paralysis with symptomatic respiratory compromise, surgical diaphragmatic plication may be considered. This procedure involves suturing or plicating the paralyzed hemidiaphragm to reduce its paradoxical movement and improve lung function.
- Phrenic Nerve Repair or Stimulation: Surgical repair of injured phrenic nerves or phrenic nerve stimulation with implantable devices may be explored in selected cases to restore diaphragmatic function and improve respiratory mechanics.
Management of Underlying Conditions:
- Identifying and treating the underlying cause of diaphragmatic paralysis is essential for optimal management. This may involve addressing neurological disorders, trauma, infections, or inflammatory conditions contributing to the paralysis.
- For idiopathic cases of diaphragmatic paralysis, symptomatic management and supportive care may be provided to alleviate respiratory symptoms and optimize patient comfort.
Symptomatic Treatment:
- Oxygen Therapy: Supplemental oxygen therapy may be administered to improve oxygenation and relieve symptoms of hypoxemia.
- Bronchodilators: In patients with underlying obstructive lung disease, bronchodilator medications may help relieve bronchospasm and improve airflow.
Pulmonary Rehabilitation:
- Pulmonary rehabilitation programs, including exercise training, education, and psychosocial support, may benefit patients with diaphragmatic paralysis by improving respiratory muscle function, exercise tolerance, and quality of life.
Monitoring and Follow-Up:
- Regular monitoring of respiratory function, symptoms, and response to treatment is essential to assess the effectiveness of interventions and adjust management strategies as needed.
- Long-term follow-up is necessary to monitor for complications, optimize respiratory support, and ensure ongoing management of the underlying condition.