Cardiomyopathy
content of this page
1- Introduction
2- Physiological Overview
3- Symptoms
4- Treatment
Introduction
Physiological Overview
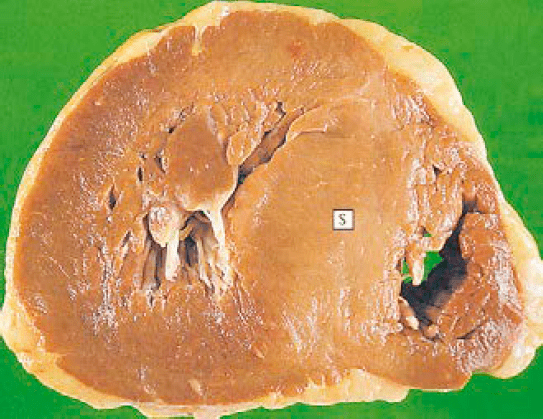
Cardiomyopathy encompasses a group of conditions that affect the heart muscle, altering its structure and function. The heart muscle, known as myocardium, becomes abnormally thickened, enlarged, or stiffened, impairing its ability to pump blood efficiently throughout the body. This dysfunction can lead to symptoms like fatigue, shortness of breath, and swelling due to fluid retention. There are several types of cardiomyopathy, including dilated cardiomyopathy, where the heart chambers enlarge and weaken; hypertrophic cardiomyopathy, characterized by abnormal thickening of the heart muscle; and restrictive cardiomyopathy, where the heart muscle becomes rigid and less compliant. These conditions can arise from genetic factors, infections, certain medications, or other underlying health issues. Physiologically, cardiomyopathy disrupts the heart’s pumping action, compromising its ability to deliver oxygenated blood to tissues and organs effectively. Management typically involves medications to improve heart function, lifestyle changes, and in some cases, procedures like implantation of devices or even heart transplantation for severe cases. Early detection and treatment are crucial in managing cardiomyopathy and preventing complications such as heart failure or arrhythmias.

Symptoms
Shortness of breath (dyspnea): This can occur during physical activity or even at rest, due to the heart’s reduced ability to pump blood effectively.
Fatigue: Feeling unusually tired or weak, even with normal activities, is a frequent symptom of cardiomyopathy.
Swelling (edema): Fluid retention can cause swelling in the legs, ankles, feet, or abdomen, as the heart struggles to pump blood efficiently.
Chest pain or discomfort: This may occur if the heart muscle is not receiving enough oxygen-rich blood.
Palpitations: Irregular heartbeats or a sensation of fluttering in the chest can occur due to abnormal heart rhythms (arrhythmias) associated with cardiomyopathy.
Dizziness or lightheadedness: Reduced blood flow to the brain can lead to feelings of dizziness or fainting.
Coughing or wheezing: Fluid buildup in the lungs (pulmonary congestion) can cause coughing, especially when lying down.
Treatment
Medications:
- Heart failure medications: Such as ACE inhibitors, beta-blockers, or angiotensin receptor blockers (ARBs) to reduce symptoms and improve heart function.
- Diuretics: To help reduce fluid buildup and swelling.
- Antiarrhythmic medications: To manage irregular heart rhythms that may accompany cardiomyopathy.
Lifestyle modifications:
- Dietary changes: Such as reducing salt intake to manage fluid retention.
- Regular exercise: As recommended by a healthcare provider to improve cardiovascular fitness.
- Quitting smoking and limiting alcohol intake.
Implantable devices:
- Implantable cardioverter-defibrillator (ICD): To monitor heart rhythm and deliver shocks if dangerous arrhythmias occur.
- Cardiac resynchronization therapy (CRT): Uses a special pacemaker to coordinate the contractions of the heart’s ventricles.
Surgical procedures:
- Septal myectomy: For hypertrophic cardiomyopathy, where part of the thickened heart muscle is removed.
- Heart transplantation: In severe cases where other treatments are not effective.
Genetic counseling and testing: For certain types of cardiomyopathy with a genetic component, counseling can help individuals understand their risk and make informed decisions about family planning and screening.
Regular monitoring:
- Ongoing medical care and regular check-ups to monitor heart function, adjust medications as needed, and detect any complications early.