Pericarditis
content of this page
1- Introduction
2- Physiological Overview
3- Symptoms
4- Treatment
Introduction
Physiological Overview
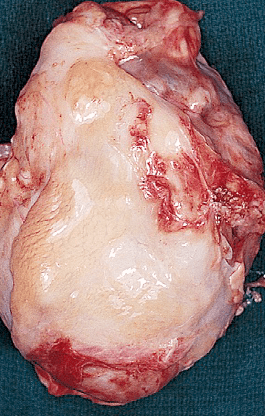
It often results from a viral infection, though it can also be caused by bacterial infections, autoimmune diseases, heart surgery, or chest trauma. Other symptoms may include fever, fatigue, and shortness of breath. While many cases resolve on their own or with anti-inflammatory medications, severe instances might require more intensive treatments to prevent complications like pericardial effusion or chronic pericarditis. Acute pericarditis is most often idiopathic or caused by viral infections such as coxsackievirus, influenzavirus, hepatitis, measles, mumps, or varicella viruses. It is also the most common cardiovascular complication of human immunodeficiency virus (HIV) infection. Other causes include myocardial infarction, trauma, neoplasm, surgery, bacterial infection (especially tuberculosis), connective tissue disease, or radiation therapy. The pericardial membranes become inflamed and roughened, and a pericardial effusion may develop that can be serous, purulent, or fibrinous. In some individuals, a large effusion can develop rapidly, causing cardiac tamponade. In most individuals, an effusion accumulates slowly and in lesser amounts that can recur in up to 30% of individuals, and can rarely progress to constrictive pericarditis.
Symptoms
- Chest Pain: Sharp, stabbing pain behind the breastbone or in the left side of the chest, which may spread to the shoulders, neck, or back. The pain often worsens with deep breathing, coughing, or lying down and improves when sitting up and leaning forward.
- Fever: A low-grade fever is common, especially if the cause is an infection.
- Shortness of Breath: Difficulty breathing, especially when lying down.
- Heart Palpitations: Sensation of rapid, fluttering, or pounding heartbeats.
- Fatigue: General feeling of weakness or tiredness.
- Cough: A dry cough may be present.
- Swelling: Swelling in the abdomen or legs, or less commonly, the arms.
Treatment
Medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Such as ibuprofen or aspirin, are commonly used to reduce inflammation and relieve pain.
- Colchicine: This anti-inflammatory medication may be used in combination with NSAIDs to prevent recurrence.
- Corticosteroids: In cases where NSAIDs are ineffective or contraindicated, corticosteroids like prednisone may be prescribed to reduce inflammation.
Treatment of Underlying Cause: If pericarditis is due to an infection (viral or bacterial), appropriate antibiotics or antiviral medications will be prescribed.
Pain Management: Analgesics may be used to alleviate chest pain if NSAIDs alone are insufficient.
Monitoring and Rest: It’s important to monitor the patient’s condition closely, especially for signs of complications such as cardiac tamponade. Rest may be recommended during the acute phase to minimize strain on the heart.
Pericardiocentesis: In cases of significant pericardial effusion causing cardiac tamponade, a procedure called pericardiocentesis may be performed to drain excess fluid from around the heart.
Follow-Up: Regular follow-up visits with a healthcare provider are important to monitor progress, adjust medications, and prevent recurrence.