Achalasia
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
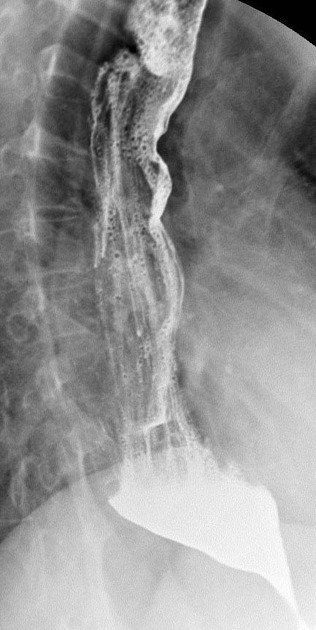
Achalasia is a rare disorder related to denervation of smooth muscle in the middle and lower portions of the esophagus, and failure of the lower esophageal sphincter (LES) to relax causing functional obstruction of the lower esophagus. Achalasia results from an unknown cause of an autoimmune destruction of myenteric ganglion cells and atrophy of smooth muscle cells. Food accumulates above the obstruction, distends the esophagus, and causes dysphagia. As hydrostatic pressure increases, food is slowly forced past the obstruction into the stomach.
Pathophysiology
Achalasia is a disorder primarily characterized by dysfunction of the esophagus, particularly involving the lower esophageal sphincter (LES) and the esophageal body. The pathophysiology of achalasia involves several key mechanisms:
Failure of Lower Esophageal Sphincter Relaxation: Normally, the LES relaxes to allow food and liquids to pass from the esophagus into the stomach. In achalasia, there is incomplete or absent relaxation of the LES, which remains contracted and fails to open adequately during swallowing.
Loss of Esophageal Peristalsis: In addition to LES dysfunction, there is a loss of peristalsis in the esophageal body. Peristalsis refers to the coordinated wave-like contractions of smooth muscle that propel food down the esophagus. This loss of peristalsis further impairs the ability of the esophagus to move food towards the stomach.
Neuronal Degeneration: The exact cause of achalasia is not fully understood, but it is believed to involve degeneration of the nerves in the esophageal wall, particularly those of the myenteric plexus (Auerbach’s plexus). This plexus plays a crucial role in coordinating the smooth muscle contractions necessary for swallowing and esophageal motility. The degeneration of these nerves leads to the dysfunction observed in achalasia.
Increased LES Pressure: Despite impaired relaxation, the LES often exhibits increased resting tone or pressure in achalasia. This high-pressure zone contributes to the difficulty in food passage from the esophagus into the stomach.
Loss of Inhibitory Neurons: The myenteric plexus normally contains inhibitory neurons that release neurotransmitters like nitric oxide and vasoactive intestinal peptide (VIP), which help to relax smooth muscle and facilitate peristalsis. In achalasia, the loss of these inhibitory neurons results in unopposed contraction of the LES and impaired esophageal peristalsis.
Symptoms
Achalasia presents with a distinct set of symptoms related to the dysfunction of the esophagus. These symptoms typically develop gradually and may vary in severity among individuals. The main symptoms of achalasia include:
Dysphagia: This is the most common and prominent symptom of achalasia. Dysphagia refers to difficulty swallowing, particularly with solid foods. Patients often describe a sensation of food sticking or getting stuck in the chest or throat. Initially, dysphagia may be mild and intermittent but can progress over time.
Regurgitation of Food: Due to impaired emptying of the esophagus, undigested food and saliva may regurgitate or come back up into the throat or mouth after eating. Regurgitation is often effortless and can occur immediately after meals or even hours later.
Chest Pain/Discomfort: Some individuals with achalasia experience chest pain or discomfort, which can be mistaken for heart-related issues (angina). The pain is typically located behind the sternum (breastbone) and may worsen after eating.
Weight Loss: Persistent dysphagia and regurgitation can lead to unintentional weight loss over time. This weight loss may be significant in cases where symptoms are severe and food intake is compromised.
Heartburn: Although less common than in gastroesophageal reflux disease (GERD), some individuals with achalasia may experience occasional heartburn or acid reflux symptoms due to impaired clearance of acidic contents from the esophagus.
Difficulty Burping: The inability to effectively release air from the stomach through burping is another symptom of achalasia. This can lead to feelings of bloating or discomfort after meals.
Coughing/Wheezing: Aspiration of regurgitated food or liquids into the lungs can occasionally cause coughing or wheezing, especially when lying down.
Treatment
The treatment of achalasia aims to relieve symptoms, improve esophageal emptying, and prevent complications associated with the disorder. The approach to treatment typically involves both non-surgical and surgical options, tailored to the individual patient’s condition and preferences. Here are the main treatment modalities for achalasia:
Non-Surgical Treatment Options:
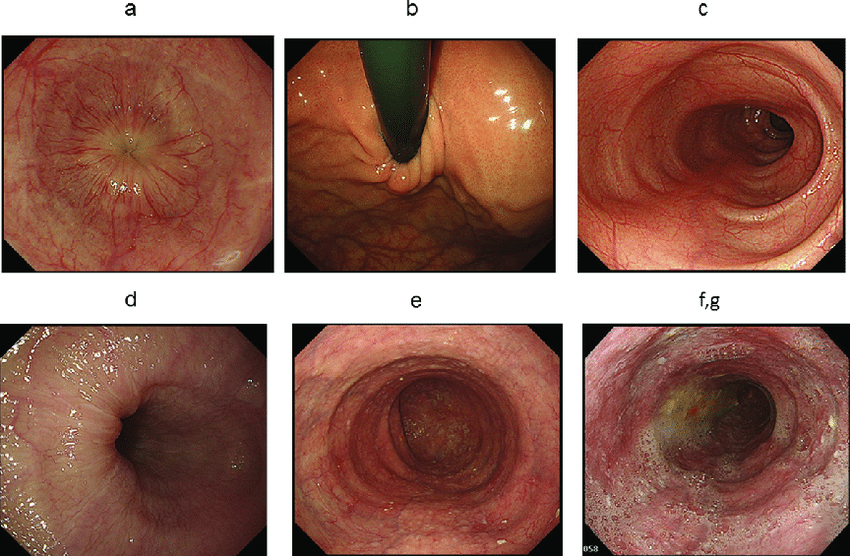
a. Pneumatic Dilation (PD): This is a common non-surgical treatment for achalasia. It involves using a balloon to stretch and widen the lower esophageal sphincter (LES) during an endoscopic procedure. The goal is to disrupt the muscle fibers of the LES and improve its ability to relax, thereby easing the passage of food into the stomach. PD is effective in many cases and can provide long-term relief, although some patients may require repeat dilations over time.
b. Botulinum Toxin Injection: In cases where pneumatic dilation is not suitable or effective, botulinum toxin (Botox) can be injected directly into the LES during an endoscopic procedure. Botox temporarily paralyzes the muscles of the LES, allowing it to relax and facilitate easier passage of food. However, the effects of Botox injections are temporary and typically last for several months, after which repeat injections may be necessary.
c. Medications: Calcium channel blockers or nitrates may be prescribed to help relax the LES and improve esophageal emptying. However, these medications are generally less effective compared to other treatments and are often used as adjunctive therapy or in patients who are not candidates for more definitive treatments.
Surgical Treatment:
a. Heller Myotomy: This is the most effective and definitive surgical treatment for achalasia. During a Heller myotomy, the surgeon cuts the muscle fibers of the LES to weaken its contraction and allow for better relaxation during swallowing. This procedure can be performed through traditional open surgery or laparoscopically (minimally invasive surgery), which typically involves smaller incisions and faster recovery times.
b. Peroral Endoscopic Myotomy (POEM): POEM is a relatively newer minimally invasive procedure that is performed entirely through an endoscope inserted through the mouth into the esophagus. The surgeon creates a myotomy (cutting of muscle fibers) similar to Heller myotomy but from inside the esophagus. POEM has shown promising results and is becoming more widely adopted as an alternative to traditional surgery.
Post-Treatment Management:
After undergoing pneumatic dilation, Botox injections, or surgery, patients with achalasia may require ongoing monitoring and management to ensure symptoms remain controlled and to address any complications that may arise. This may include dietary adjustments to accommodate swallowing difficulties and regular follow-up visits to assess esophageal function.