Diabetes Mellitus
content of this page
1- Introduction
2- Physiological Overview
3- Symptoms
4- Treatment
Introduction

Physiological Overview
Diabetes mellitus (DM) is a metabolic disorder characterized by chronic hyperglycemia, or high blood sugar levels, resulting from defects in insulin production, insulin action, or both. Insulin, produced by the beta cells of the pancreas, plays a pivotal role in regulating glucose metabolism. In type 1 diabetes, an autoimmune condition, the immune system attacks and destroys these insulin-producing cells, leading to an absolute insulin deficiency. Type 2 diabetes, the most common form, typically develops when the body becomes resistant to insulin or when the pancreas fails to produce enough insulin to meet the body’s demands. Insulin resistance means that the body’s cells do not respond effectively to insulin, leading to reduced glucose uptake from the bloodstream. As a result, glucose accumulates in the blood, causing hyperglycemia. Over time, chronic hyperglycemia can damage blood vessels and nerves, increasing the risk of complications such as cardiovascular disease, kidney disease, neuropathy, and vision problems.
Symptoms
Polyuria: Increased urination occurs as the kidneys attempt to rid the body of excess glucose.
Polydipsia: Excessive thirst results from the body’s effort to compensate for fluid loss through frequent urination.
Polyphagia: Increased hunger can occur, especially in type 1 diabetes, as the body seeks fuel due to the inability to use glucose effectively.
Weight loss: Unintended weight loss may occur in type 1 diabetes, despite increased appetite, due to the body breaking down muscle and fat for energy.
Fatigue: Feeling tired and lethargic is common as cells are deprived of glucose, their primary source of energy.
Blurred vision: High blood sugar levels can cause fluid to be pulled from the lenses of the eyes, affecting the ability to focus clearly.
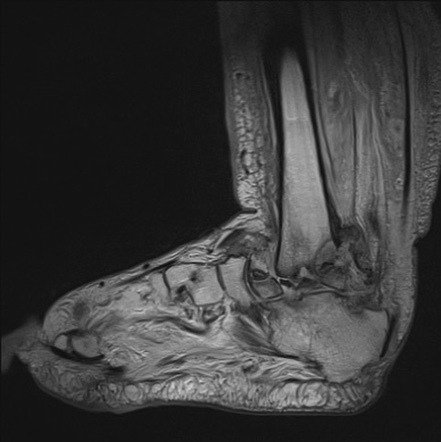
Slow wound healing: High blood sugar impairs the body’s ability to heal wounds and injuries.
Recurrent infections: People with diabetes are more susceptible to infections, especially yeast infections (such as thrush) and urinary tract infections.
Numbness or tingling in hands or feet: This can be a sign of nerve damage (neuropathy) caused by prolonged high blood sugar levels.
Dry, itchy skin: High blood sugar can cause dehydration, leading to dry skin and itchiness.
Treatment
Lifestyle Modifications:
- Healthy Diet: A balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats helps regulate blood sugar levels. Monitoring carbohydrate intake is particularly important.
- Regular Exercise: Physical activity improves insulin sensitivity and helps lower blood sugar levels. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, along with strength training exercises.
Medications:
- Insulin Therapy: People with type 1 diabetes and some with type 2 diabetes require insulin injections or insulin pump therapy to replace the insulin their bodies no longer produce or use effectively.
- Oral Medications: For type 2 diabetes, various classes of oral medications may be prescribed to improve insulin sensitivity, reduce glucose production by the liver, or increase insulin secretion from the pancreas.
Blood Sugar Monitoring:
- Regular monitoring of blood glucose levels helps individuals with diabetes and their healthcare providers adjust treatment plans as needed. This may involve self-monitoring at home with a blood glucose meter or continuous glucose monitoring (CGM) systems.
Education and Support:
- Diabetes self-management education (DSME) provides knowledge and skills to effectively manage diabetes, including understanding medications, monitoring blood sugar, making dietary choices, and managing stress.
- Support from healthcare providers, diabetes educators, and support groups can help individuals cope with the challenges of diabetes and adhere to their treatment plans.
Management of Cardiovascular Risk Factors:
- Managing blood pressure and cholesterol levels is crucial, as people with diabetes are at higher risk for cardiovascular disease. This may involve medications, lifestyle changes, and regular monitoring.
Regular Medical Care:
- Routine medical visits allow for monitoring of overall health, screening for complications, and adjustments to treatment plans as needed.
Preventive Care:
- Preventive measures include vaccinations (such as flu and pneumococcal vaccines), regular eye exams (to detect diabetic retinopathy), foot care (to prevent complications like neuropathy and ulcers), and dental care.