Hashimoto's Thyroiditis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
Hashimoto’s thyroiditis is an autoimmune disease where the body’s immune system mistakenly targets and damages the thyroid gland, leading to inflammation and reduced thyroid hormone production. This can cause the thyroid to become enlarged (goiter) and result in hypothyroidism, a condition where the thyroid does not produce enough hormones.
Causes
1. Genetic Predisposition:
- Family History: Having a family history of autoimmune thyroid disease or other autoimmune disorders increases the risk of developing Hashimoto’s thyroiditis.
2. Gender:
- Higher Risk in Women: Women are more likely to develop Hashimoto’s thyroiditis compared to men, suggesting hormonal factors may play a role.
3. Autoimmune Conditions:
- Associated Conditions: Individuals with other autoimmune disorders, such as type 1 diabetes, rheumatoid arthritis, or lupus, are at a higher risk.
4. Environmental Triggers:
- Infections: Certain viral or bacterial infections might trigger the autoimmune response.
- Stress: Physical or emotional stress can potentially contribute to the onset or worsening of autoimmune conditions.
5. Iodine Intake:
- Excessive or Deficient Iodine: Both very high and very low iodine levels can affect thyroid function and might be linked to autoimmune thyroid disease.
6. Hormonal Changes:
- Pregnancy and Postpartum: Hormonal changes during and after pregnancy can sometimes trigger Hashimoto’s thyroiditis in susceptible individuals.
7. Radiation Exposure:
- Radiation Therapy: Prior radiation treatment, especially to the head or neck area, can increase the risk of developing thyroid problems, including Hashimoto’s thyroiditis.
8. Other Factors:
- Certain Medications: Long-term use of some medications, such as lithium, can affect thyroid function and potentially trigger autoimmune thyroiditis.
Symptoms
-General Symptoms:
- Fatigue: Persistent tiredness and low energy levels.
- Weight Gain: Unexplained weight gain despite normal eating habits.
- Cold Intolerance: Sensitivity to cold temperatures, feeling unusually cold.
- Constipation: Difficulty passing stools and reduced bowel movements.
-Skin and Hair:
- Dry Skin: Rough, dry skin that may feel itchy.
- Hair Loss: Thinning hair or loss of hair, particularly on the scalp.
- Pale or Yellowish Skin: A noticeable change in skin color.
-Musculoskeletal Symptoms:
- Muscle Weakness: General weakness, particularly in the legs and arms.
- Joint Pain: Aching or stiffness in the joints.
-Cognitive and Mood Changes:
- Depression: Feelings of sadness or depression.
- Memory Problems: Difficulty with concentration and memory.
-Digestive Issues:
- Constipation: Slower bowel movements and difficulty passing stools.
-Cardiovascular Symptoms:
- Slow Heart Rate: A lower than normal heart rate (bradycardia).
- Elevated Cholesterol: Increased levels of cholesterol in the blood.
-Reproductive Symptoms:
- Irregular Menstrual Cycles: Changes in menstrual periods, such as heavier or more frequent bleeding.
- Difficulty Conceiving: Problems with fertility in women.
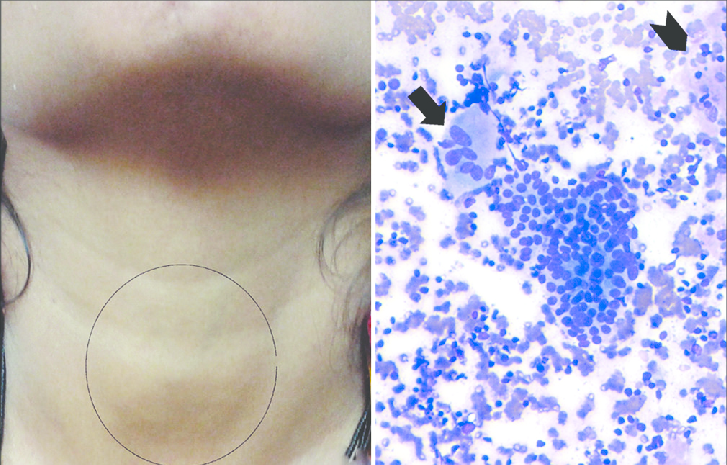
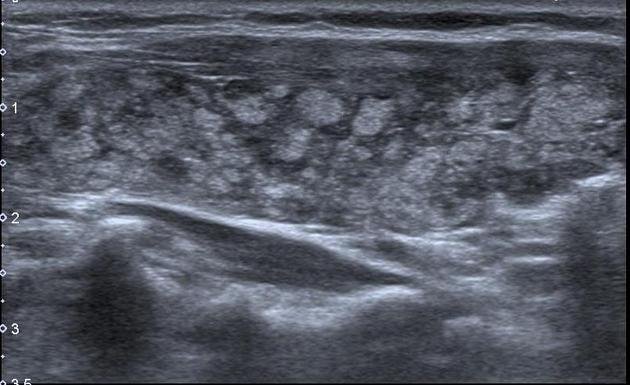
-Goiter (Enlarged Thyroid):
- Swelling in the Neck: Visible enlargement of the thyroid gland in the neck, which can cause a swelling or lump.
-Other Symptoms:
- Muscle Cramps: Unexplained muscle cramps or stiffness.
- Hoarseness: Changes in voice, such as hoarseness or a deepened voice
Stages of The Disease
1. Early Stage (Subclinical Hypothyroidism):
- Symptoms: Mild or no noticeable symptoms. Thyroid hormone levels may be normal or slightly reduced, while thyroid-stimulating hormone (TSH) levels may be elevated.
- Diagnosis: Often detected through routine blood tests showing elevated TSH levels but normal thyroid hormone levels.
2. Progressive Hypothyroidism:
- Symptoms: More pronounced symptoms of hypothyroidism begin to appear, such as fatigue, weight gain, cold intolerance, and constipation.
- Diagnosis: Blood tests show elevated TSH levels and reduced levels of thyroid hormones (T3 and T4). The thyroid gland may become enlarged (goiter).
3. Established Hypothyroidism:
- Symptoms: Full-blown symptoms of hypothyroidism become evident and can include severe fatigue, significant weight gain, dry skin, hair loss, and cognitive issues.
- Diagnosis: Blood tests confirm reduced thyroid hormone levels and high TSH levels. The thyroid gland might continue to enlarge if the disease progresses without treatment.
4. Complications and Long-Term Management:
- Symptoms: Ongoing symptoms of hypothyroidism may persist or worsen if not properly managed. Potential complications include cardiovascular issues, severe depression, and infertility.
- Management: Lifelong thyroid hormone replacement therapy is required to manage symptoms and maintain normal thyroid function. Regular monitoring of thyroid hormone levels and adjustment of medication is essential.
5. Advanced Cases (Rare):
- Symptoms: In rare cases, untreated or poorly managed Hashimoto’s thyroiditis can lead to severe complications like myxedema coma, a life-threatening condition characterized by extreme hypothyroidism.
- Management: Immediate medical intervention is required. This stage is less common with proper treatment and monitoring.
Treatment
1. Thyroid Hormone Replacement Therapy:
- Levothyroxine: The most commonly prescribed medication is levothyroxine, a synthetic form of thyroid hormone (T4). It helps normalize thyroid hormone levels and alleviate symptoms of hypothyroidism.
- Dosage: The dosage is adjusted based on regular blood tests to monitor thyroid hormone levels (T3, T4) and thyroid-stimulating hormone (TSH).
2. Regular Monitoring:
- Blood Tests: Regular blood tests are required to monitor thyroid hormone levels and adjust medication dosage as needed.
- Follow-Up: Regular follow-up appointments with a healthcare provider are essential to ensure effective management and address any emerging symptoms or issues.
3. Dietary and Lifestyle Adjustments:
- Balanced Diet: Eating a balanced diet rich in fruits, vegetables, lean proteins, and whole grains can support overall health.
- Avoiding Certain Foods: While there’s no strict diet for Hashimoto’s, some individuals may benefit from avoiding excessive amounts of soy products or gluten if they experience sensitivities.
- Regular Exercise: Engaging in regular physical activity can help manage weight and improve overall well-being.
4. Managing Symptoms:
- Addressing Specific Issues: Symptoms such as joint pain, dry skin, or hair loss may require additional treatments or therapies. For example, moisturizing creams for dry skin or medications for joint pain.
- Mental Health Support: Therapy or counseling may be beneficial for managing depression or anxiety related to chronic illness.
5. Treating Associated Conditions:
- Autoimmune Support: If there are other autoimmune conditions present, they should be managed according to their specific treatment protocols.
6. Surgery (Rare):
- Thyroidectomy: In rare cases, if there is a large goiter causing symptoms or compression, surgical removal of part or all of the thyroid gland may be considered. This would generally be followed by lifelong thyroid hormone replacement therapy.
7. Patient Education:
- Understanding the Condition: Educating patients about Hashimoto’s thyroiditis, its symptoms, and treatment options helps them manage their condition effectively.
- Emergency Preparedness: Knowing when and how to seek medical help, especially if symptoms worsen or if there are signs of an acute condition like myxedema coma.
What Should You Avoid
1. Excessive Iodine:
- High-Iodine Foods: Avoid excessive consumption of iodine-rich foods or supplements, as too much iodine can affect thyroid function. Foods like seaweed and certain iodized salts should be consumed in moderation.
2. Goitrogenic Foods (In Moderation):
- Raw Cruciferous Vegetables: Foods like broccoli, cauliflower, kale, and cabbage contain goitrogens, which can interfere with thyroid function. Cooking these vegetables usually reduces their goitrogenic effect, so they can be eaten in moderation when cooked.
3. Soy Products:
- Soy and Thyroid Medication: Excessive consumption of soy products can interfere with thyroid hormone absorption. If you consume soy, try to space it out from your thyroid medication.
4. Gluten (If Sensitive):
- Gluten Sensitivity: Some people with Hashimoto’s thyroiditis may also have gluten sensitivity or celiac disease. If gluten exacerbates your symptoms, consider a gluten-free diet.
5. Stress:
- High Stress: Chronic stress can negatively impact thyroid function and overall health. Managing stress through relaxation techniques, exercise, and counseling can be beneficial.
6. Smoking and Excessive Alcohol:
- Smoking: Smoking can worsen autoimmune conditions and affect overall health.
- Excessive Alcohol: Heavy alcohol consumption can interfere with thyroid hormone absorption and overall health.
7. Certain Medications:
- Interactions: Be cautious with medications that can interfere with thyroid function or thyroid hormone absorption. Always inform your healthcare provider about all the medications and supplements you are taking.
8. Extreme Dietary Changes:
- Unbalanced Diet: Avoid extreme dietary changes or fad diets that can lead to nutritional deficiencies or imbalances, affecting overall health and thyroid function.
9. Neglecting Regular Check-Ups:
- Missed Appointments: Regular monitoring and follow-up with your healthcare provider are essential to adjust medication and manage the condition effectively.
10. Self-Medication:
- Avoid Unsupervised Changes: Never adjust your thyroid medication or try alternative treatments without consulting your healthcare provider, as this can disrupt your thyroid function and overall health.