Hyperparathyroidism
content of this page
1- Introduction
2- Pathophysiological Overview
3- Symptoms
4- Treatment
Introduction
of hyperparathyroidism are classified as either primary or secondary, and their associated pathophysiologic mechanisms are somewhat different.
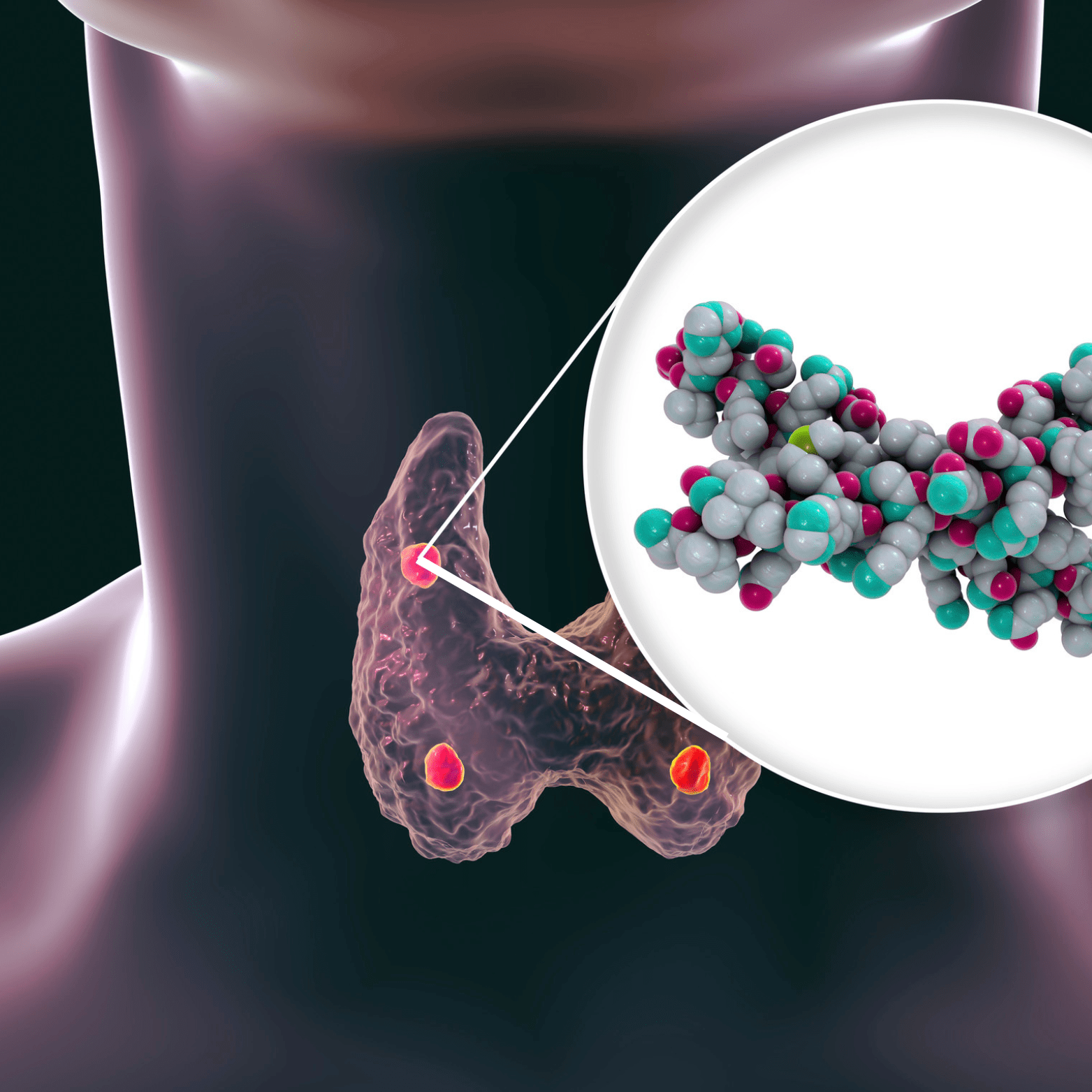
Pathophysiological Overview
Primary hyperparathyroidism is characterized by inappropriate excess secretion of PTH by one or more of the parathyroid glands. It is one of the most common endocrine disorders: 80% to 85% of cases are Primary hyperparathyroidism is caused by parathyroid adenomas in about 85% of cases, with another 10% to 15% resulting from parathyroid hyperplasia, and approximately 1% caused by parathyroid carcinoma. In primary hyperparathyroidism, normal feedback mechanisms, such as elevated serum levels of ionized calcium, fail to normally inhibit PTH secretion by the parathyroid gland.
Secondary hyperparathyroidism is caused by an increase in PTH secondary to a chronic disease state, such as chronic renal failure or intestinal malabsorption, which leads to a decrease in serum ionized calcium levels (hypocalcemia). Hypercalcemia does not occur in secondary hyperparathyroidism because the parathyroid tissue is not autonomous and is only responding to a physiologic stimulus (hypocalcemia).
Symptoms
- Fatigue: Feeling tired or lacking energy.
- Weakness: Reduced strength, particularly in muscles.
- Bone Pain: Aching bones, often in the back, hips, or ribs.
- Kidney Stones: Formation of kidney stones due to elevated calcium levels.
- Frequent Urination: Increased need to urinate.
- Digestive Issues: Constipation or abdominal discomfort.
- Cognitive Changes: Difficulty concentrating or memory problems.
- Depression: Feeling sad or low in mood.
- Bone Fractures: Increased risk of fractures due to weakened bones (osteoporosis).
- High Blood Pressure: Elevated blood pressure in some cases.
Treatment
Observation and Monitoring: For mild cases without symptoms, periodic monitoring of calcium levels and symptoms may be recommended.
Surgery (Parathyroidectomy):
- Primary Hyperparathyroidism: Surgical removal of the abnormal parathyroid gland(s) (adenoma, hyperplasia, or carcinoma) is often the preferred treatment, especially if symptoms are severe or complications like kidney stones or osteoporosis are present.
- Secondary Hyperparathyroidism: Surgery may be considered in some cases, particularly if medical management fails or if there is severe hypercalcemia or complications.
Medication:
- Calcimimetics: These drugs mimic the action of calcium on the parathyroid glands and can help lower PTH levels.
- Bisphosphonates: These medications are used to treat osteoporosis associated with hyperparathyroidism by slowing down bone loss.
Management of Complications:
- Treatment of kidney stones, osteoporosis, and other complications associated with hyperparathyroidism may also be necessary.
Addressing Underlying Causes:
- For secondary hyperparathyroidism, treating the underlying condition (e.g., renal failure, vitamin D deficiency) is essential to manage PTH levels.