Kallmann Syndrome
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Investigations & Lab Results
5- Prognosis
6- Treatment
Introduction
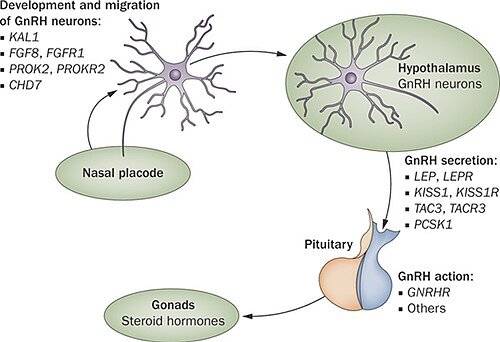
Kallmann Syndrome is a rare genetic disorder that primarily affects the development of the reproductive system and the sense of smell. It is characterized by hypogonadotropic hypogonadism, a condition in which the body fails to start or fully complete puberty due to a deficiency of gonadotropin-releasing hormone (GnRH), and anosmia or hyposmia, which is the absence or reduced ability to smell. This syndrome results from the failure of GnRH-producing neurons to migrate properly to the hypothalamus during embryonic development, often due to mutations in various genes such as ANOS1, FGFR1, or PROKR2
Causes
-Genetic Causes
Several gene mutations have been associated with Kallmann Syndrome. These include:
ANOS1 (formerly KAL1) – Located on the X chromosome; causes X-linked Kallmann Syndrome, primarily affecting males.
FGFR1 and FGF8 – Mutations affect the development of olfactory and GnRH neurons; usually inherited in an autosomal dominant pattern.
PROK2 and PROKR2 – Involved in neuron signaling and migration; can be inherited in autosomal dominant or recessive patterns.
CHD7, SOX10, and others – Associated with syndromic forms of KS, such as CHARGE syndrome.
In many cases, the exact gene mutation cannot be identified, and the condition may appear sporadically without a clear family history.
-Inheritance Patterns
X-linked: Seen with ANOS1 mutations, typically affects males.
Autosomal dominant: A single copy of the mutated gene can cause the disorder.
Autosomal recessive: Both copies of the gene must be mutated for the condition to manifest.
Symptoms
-Main Symptoms
Delayed or absent puberty
Males: Lack of testicular enlargement, low testosterone levels, absence of facial/body hair, voice not deepening, underdeveloped muscles.
Females: Lack of breast development, absence of menstruation (primary amenorrhea), low estrogen levels.
Anosmia or hyposmia
Complete or partial loss of the sense of smell, often unnoticed until puberty is delayed and investigated.
Infertility
Due to lack of sex hormone production and impaired sperm or egg development.
-Additional Possible Symptoms
Micropenis and undescended testes (cryptorchidism) – in males, due to low testosterone during fetal development.
Cleft lip and/or palate
Hearing loss
Color blindness
Mirror movements (synkinesis) – involuntary movements on one side of the body that mirror voluntary movements on the other.
Kidney abnormalities – such as a missing kidney (renal agenesis).
Facial asymmetry or midline facial defects
Dental anomalies – delayed tooth eruption or missing teeth.
Investigations & Lab Results
GnRH ↓ (low or absent due to hypothalamic deficiency)
LH ↓ or → (low or inappropriately normal)
FSH ↓ or → (low or inappropriately normal)
Testosterone (in males) ↓
Estradiol (in females) ↓
Prolactin → (normal)
TSH and Free T4 → (normal, helps rule out thyroid-related causes)
Bone age ↓ (delayed compared to chronological age)
Semen analysis (in males) ↓ (low sperm count or azoospermia)
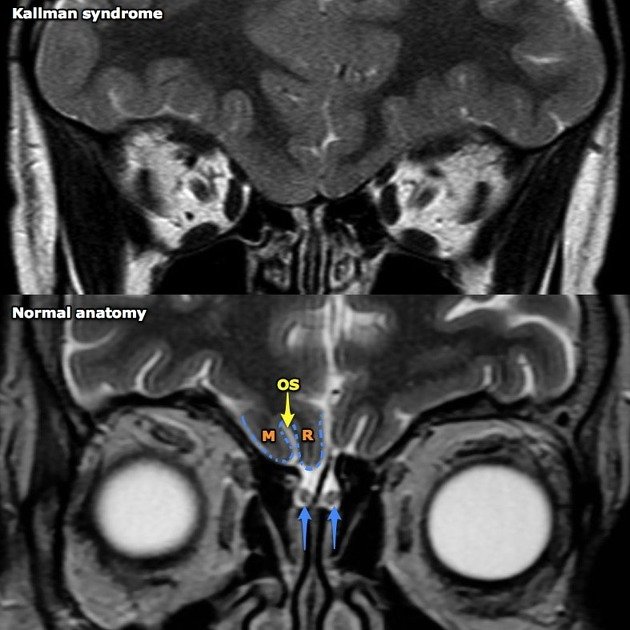
MRI of brain/olfactory bulbs →/absent (normal pituitary, often absent or underdeveloped olfactory bulbs)
Olfactory test (smell test) ↓ or absent (anosmia or hyposmia)
GnRH stimulation test response ↓ (blunted LH/FSH response)
Prognosis
Puberty and Sexual Development: Hormone replacement therapy (testosterone in males, estrogen/progesterone in females) can successfully induce and maintain secondary sexual characteristics.
Fertility: Although natural fertility is impaired due to lack of GnRH, fertility can often be achieved with specialized treatment such as pulsatile GnRH therapy or gonadotropin injections to stimulate sperm or egg production.
Sense of Smell: Loss of smell (anosmia or hyposmia) is typically permanent, as it is due to structural brain abnormalities like absent olfactory bulbs.
Psychosocial Impact: Delayed puberty and infertility can lead to emotional or psychological challenges, but early support, counseling, and education can improve quality of life.
Spontaneous Reversal: In a small number of cases (estimated 10–20%), spontaneous recovery of GnRH secretion may occur later in life, but continued monitoring is necessary to assess hormone levels and sexual function.
Treatment
1. Hormone Replacement Therapy (HRT)
Used to induce and maintain secondary sexual characteristics.
Males:
Testosterone (injectable, gel, patch, or oral):
Initiates and maintains features such as facial hair, deep voice, muscle mass, and libido.
Females:
Estrogen (initially) → followed by combined estrogen-progesterone therapy:
Promotes breast development, menstruation, and uterine growth.
2. Fertility Treatment
For patients wishing to have children.
Pulsatile GnRH therapy:
Mimics natural GnRH release via a pump; effective for inducing ovulation or spermatogenesis.
Requires a functioning pituitary.
Gonadotropin injections:
Men: hCG (human chorionic gonadotropin) + FSH to stimulate testicular growth and sperm production.
Women: FSH + LH (or hCG) to induce ovulation.
3. Psychological and Social Support
Counseling is important, especially for adolescents facing delayed puberty or fertility concerns.
Peer support groups and educational resources can be helpful.
4. Monitoring and Follow-up
Regular follow-up to adjust hormone dosages.
Bone density monitoring (due to risk of osteoporosis from low sex hormone levels).
Periodic reassessment of reproductive function; rare cases may experience spontaneous GnRH recovery.
5. Surgical Treatment (if needed)
Cryptorchidism (undescended testes) or cleft lip/palate may require surgical correction.