Thyroid Adenoma
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Investigations & Lab Results
5- Prognosis
6- Treatment
Introduction
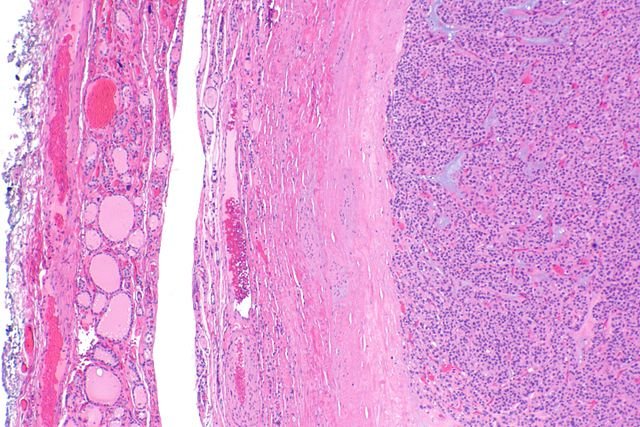
Thyroid Adenoma is a benign (non-cancerous), solitary tumor arising from the follicular cells of the thyroid gland. It is usually well-encapsulated and does not invade surrounding tissues. Most thyroid adenomas are non-functional and asymptomatic, but some can become toxic adenomas, meaning they produce thyroid hormones independently of TSH regulation, leading to hyperthyroidism.
These adenomas are often discovered incidentally during a neck examination or imaging for another reason. Though benign, they must be evaluated carefully to differentiate them from follicular thyroid carcinoma, as they can appear similar on imaging and cytology.

Causes
Somatic mutations in thyroid follicular cells (especially in the TSH receptor or GNAS gene)
Chronic stimulation by thyroid-stimulating hormone (TSH) — can promote cell proliferation
Iodine deficiency — leads to increased TSH stimulation and follicular cell growth
Radiation exposure to the head or neck during childhood
Genetic predisposition — family history of thyroid nodules or tumors
Female gender and advancing age — thyroid nodules, including adenomas, are more common in women and older adults
Symptoms
-If non-toxic (non-functioning) adenoma:
Painless, solitary thyroid nodule
Noticeable lump or swelling in the neck
Cosmetic concerns
Occasional discomfort or tightness in the neck (if large)
Rarely, difficulty swallowing or breathing (from compression of nearby structures)
-If toxic (functioning) adenoma:
Signs of hyperthyroidism, such as:
Weight loss despite normal or increased appetite
Heat intolerance
Palpitations
Tremors
Anxiety or nervousness
Menstrual irregularities
Fatigue
Increased sweating
Investigations & Lab Results
- Thyroid Function Tests:
TSH:
↓ in toxic (functioning) adenoma
→ Normal in non-functioning adenoma - Free T4 / T3:
↑ in toxic adenoma
→ Normal in non-functioning adenoma - Thyroid Antibodies:
→ Negative (helps exclude autoimmune thyroid diseases) - Thyroid Ultrasound:
→ Solitary, well-defined, encapsulated nodule
→ May show solid or cystic areas, internal vascularity - Radioactive Iodine Uptake Scan (RAIU):
↑ uptake (“hot” nodule) in toxic adenoma
↓ uptake (“cold” nodule) in non-functioning adenoma - Fine Needle Aspiration (FNA):
→ Suggests follicular neoplasm but cannot definitively distinguish adenoma from carcinoma (requires histopathology)
Prognosis
Generally excellent, as most thyroid adenomas are benign and slow-growing.
No invasion or metastasis occurs in true adenomas, which remain well-encapsulated.
Toxic adenomas causing hyperthyroidism can be effectively treated with radioactive iodine, surgery, or medications.
Rarely, a follicular adenoma may be misdiagnosed if it is actually a minimally invasive carcinoma—histopathology after surgery is definitive.
With appropriate monitoring or treatment, recurrence is rare and quality of life is unaffected in most cases.
Treatment
1. Observation
For small, non-functioning, asymptomatic adenomas
Regular monitoring with:
Physical exams
Thyroid function tests
Ultrasound
Fine-needle aspiration (FNA) if nodule changes or grows
2. Surgery (Lobectomy or Thyroidectomy)
Indicated for:
Large nodules causing pressure symptoms
Suspicion of cancer (especially follicular neoplasm on FNA)
Patient preference or cosmetic concern
Toxic adenomas not responsive to medical or RAI treatment
3. Radioactive Iodine Therapy (RAI)
Used for toxic (functioning) adenomas
Destroys hyperfunctioning thyroid tissue and controls hyperthyroidism
Less invasive than surgery
4. Antithyroid Medications
Methimazole or propylthiouracil (PTU) used short-term for toxic adenomas
Helps control symptoms before definitive treatment (RAI or surgery)
Not a long-term solution in most cases
5. Beta-Blockers
For symptomatic relief in hyperthyroid patients (e.g., palpitations, tremors)