Immune Thrombocytopenic Purpura (ITP)
Content of This Page
1- Introduction
2- Pathophysiology
3- Genetics & Inheritance
4- Clinical Features
5- Investigations
6- Treatment
7- Prognosis & Follow-up
Introduction
Immune Thrombocytopenic Purpura (ITP) is an acquired autoimmune disorder characterized by isolated thrombocytopenia (low platelet count) due to immune-mediated destruction of platelets. It may present as either an acute, self-limiting illness (especially in children) or a chronic, relapsing condition in adults.
The hallmark feature of ITP is mucocutaneous bleeding (e.g. petechiae, purpura, easy bruising), though many patients are asymptomatic. Diagnosis is one of exclusion, meaning other causes of thrombocytopenia must be ruled out.
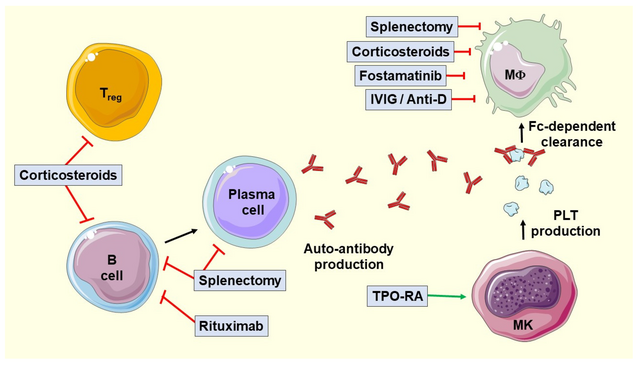
Pathophysiology
1. Autoantibody Formation
Autoantibodies (mainly IgG) are produced against glycoproteins on the platelet surface, particularly:
GpIIb/IIIa
GpIb/IX
These antibodies are usually generated by autoreactive B cells and may be triggered by infections, vaccines, or autoimmune diseases.
2. Platelet Destruction
Antibody-coated platelets are cleared by macrophages in the reticuloendothelial system, especially in the spleen.
This leads to shortened platelet lifespan, often reduced to a few hours (normal = ~7–10 days).
3. Impaired Platelet Production
In addition to peripheral destruction, autoantibodies may also target megakaryocytes in the bone marrow.
This impairs platelet production, compounding the thrombocytopenia.
4. T-Cell Dysregulation
Emerging evidence suggests a role for cytotoxic T cells, which may directly damage platelets or megakaryocytes.
There is also reduced regulatory T cell activity, contributing to immune dysregulation.

Genetics & Inheritance
1. Is ITP Inherited?
No, ITP is not directly inherited.
Most cases are sporadic and occur without a family history.
However, familial clustering has been reported, suggesting a genetic predisposition in some individuals.
2. Genetic Susceptibility Factors
Certain genetic factors may increase susceptibility to ITP or influence disease course:
| Genetic Feature | Role |
|---|---|
| HLA Class II alleles | Associated with increased risk of autoantibody production (e.g. HLA-DRB1 variants) |
| Polymorphisms in immune genes | Affect T-cell regulation and B-cell activity (e.g. CTLA-4, TNF-α) |
| Fc receptor gene variants | Influence how antibody-coated platelets are cleared |
3. Familial ITP (Rare)
Extremely rare familial forms of ITP exist, especially in paediatric cases.
May overlap with inherited thrombocytopenic syndromes, but these are usually non-immune in mechanism and require careful diagnostic distinction.
4. Related Autoimmune Background
ITP may occur more frequently in individuals with a personal or family history of autoimmune diseases, such as:
Systemic lupus erythematosus (SLE)
Autoimmune thyroid disease
Type 1 diabetes mellitus
This suggests a shared genetic susceptibility to autoimmunity, not specific inheritance of ITP itself.
Clinical Features
| System Affected | Clinical Features |
|---|---|
| Skin | Petechiae, purpura, ecchymoses |
| Mucosa | Epistaxis, gum bleeding, menorrhagia |
| GI/Urinary | Melaena, haematuria |
| CNS | Rare: headache, neurological signs (due to ICH) |
| Systemic exam | Usually normal; no splenomegaly or lymphadenopathy |
Investigations
| Purpose | Tests |
|---|---|
| Confirm isolated thrombocytopenia | FBC, blood film |
| Exclude secondary causes | HIV, HCV, ANA, H. pylori |
| Rule out mimics | Coagulation tests, bone marrow (if needed) |
| Detect associated conditions | Direct Coombs, flow cytometry (selected cases) |
Treatment
| Stage | Treatment Options |
|---|---|
| First-line | Corticosteroids, IVIG |
| Second-line | Rituximab, splenectomy, TPO agonists |
| Emergency / bleeding | IVIG + steroids ± platelets |
| Paediatric cases | Observation or IVIG/steroids if bleeding |
Prognosis & Follow-up
| Aspect | Details |
|---|---|
| Prognosis – Children | Excellent; most resolve spontaneously |
| Prognosis – Adults | Chronic course common but manageable |
| Follow-up needed | Platelets, bleeding symptoms, treatment side effects |
| Post-splenectomy | Vaccines, sepsis prevention |