Sideroblastic Anemia
Content of This Page
1- Introduction
2- Pathophysiology
3- Clinical Features (Recognize chronic clinical features)
4- Interpret labs and diagnostics
5-Management of acute complications
6- Preventive strategies
7-Indications for transfusion & transplant
8- Complications
9- Prognosis & mortality trends
Introduction
Sideroblastic anaemia is a group of disorders characterised by defective incorporation of iron into haem, leading to ineffective erythropoiesis, iron accumulation in erythroblast mitochondria, and the appearance of ring sideroblasts in bone marrow.
Pathophysiology
The defect is in haem biosynthesis, particularly at the step catalyzed by ALA synthase (ALAS2).
Iron is transported into mitochondria but not incorporated into haem, resulting in:
Ineffective red cell production
Mitochondrial iron overload
Can be:
Congenital (e.g. X-linked ALAS2 mutation)
Acquired: due to myelodysplastic syndromes (MDS), alcohol, lead, copper deficiency, or drugs (e.g. isoniazid)
Clinical Features
Often chronic microcytic anaemia with fatigue and pallor
May present with:
Splenomegaly
Iron overload signs: bronze skin, diabetes, hepatomegaly
Congenital forms present earlier; acquired forms more often in older adults
Interpret labs and diagnostics
Blood tests:
↓ Hb, ↓/N MCV (often dimorphic)
↑ Serum iron, ↑ Ferritin, ↑ Transferrin saturation
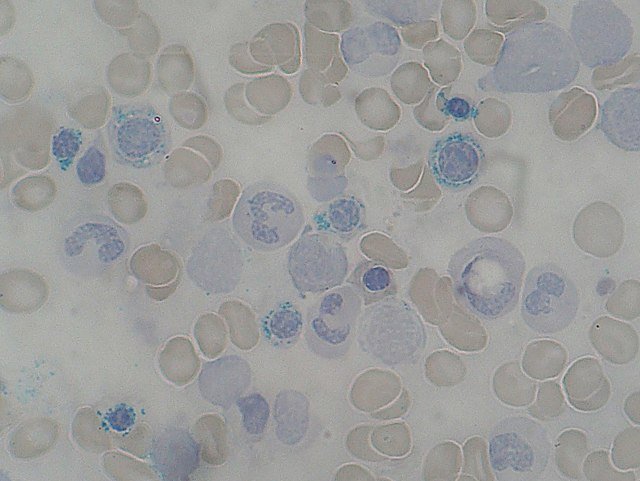
Blood film:
Basophilic stippling, target cells
Bone marrow:
Prussian blue stain shows ring sideroblasts
Consider:
Genetic testing (for congenital)
Lead levels, copper, and B6 status
Cytogenetics if MDS is suspected
Management of acute complications
Acute haemolysis or symptomatic anaemia may need blood transfusion
Manage iron overload (esp. with frequent transfusions):
Iron chelation (e.g. deferasirox)
Infections or marrow suppression → treat promptly
Preventive strategies
Avoid triggers: alcohol, toxins, offending medications
Vitamin B6 (pyridoxine) supplementation in congenital forms
Monitor and prevent iron overload in transfused patients
Indications for transfusion & transplant
Transfusion:
When anaemia becomes symptomatic or Hb critically low
Bone marrow/stem cell transplant:
Considered in refractory congenital cases or progression to MDS/leukaemia
Complications
Secondary haemochromatosis (iron overload)
Cardiomyopathy, endocrinopathies (diabetes, hypothyroidism)
In MDS-associated forms: progression to acute myeloid leukaemia (AML)
Prognosis & mortality trends
Depends on cause:
Reversible acquired forms (e.g. drug-induced) → good outcome with removal of trigger
Congenital or MDS-related forms → chronic disease, risk of progression
Monitoring for iron overload and marrow failure is essential