Thrombotic Thrombocytopenic Purpura (TTP)
Content of This Page
1- Introduction
2- Pathophysiology
3- Clinical Features
4- Investigations
5- Management
6- Differential Diagnosis
7- Complications
8- Prognosis
Introduction
TTP is a rare, life-threatening thrombotic microangiopathy (TMA) characterized by:
Thrombocytopenia
Microangiopathic haemolytic anaemia (MAHA)
Plus potential involvement of the CNS, kidneys, and fever
It is considered a medical emergency with high mortality if untreated.
Pathophysiology
TTP is primarily caused by:
Severe deficiency of ADAMTS-13 (<10% activity), due to:
Autoantibodies (acquired TTP)
Rarely inherited (congenital Upshaw–Schulman syndrome)
-Mechanism:
ADAMTS-13 normally cleaves ultra-large von Willebrand factor (vWF) multimers
Without it, vWF accumulates → platelet aggregation in microvasculature
Leads to widespread platelet-rich thrombi, especially in brain and kidneys
Clinical Features
Classic Pentad (though rarely all present together):
Thrombocytopenia (purpura, bruising)
Microangiopathic haemolytic anaemia (MAHA)
Neurological signs: confusion, seizures, stroke-like symptoms
Renal impairment: mild to moderate
Fever
-Signs of MAHA include:
Anaemia
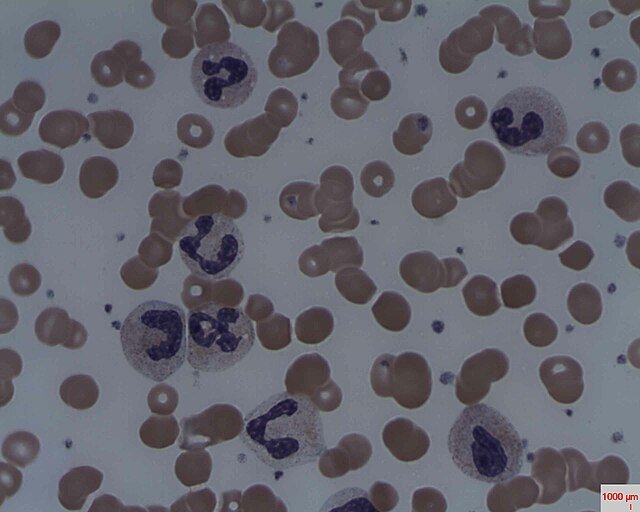
Schistocytes on blood film
↑ LDH, ↓ haptoglobin, ↑ indirect bilirubin
Investigations
FBC: ↓ Platelets, anaemia
Blood film: Schistocytes (fragmented RBCs)
Haemolysis markers: ↑ LDH, ↑ bilirubin, ↓ haptoglobin
Renal function: May be impaired
ADAMTS-13 activity: <10% diagnostic (if available)
Coombs test: Negative (distinguishes from autoimmune haemolytic anaemia)
Management
Medical emergency – start treatment urgently without waiting for ADAMTS-13 results
First-line:
Plasma exchange (PEX) – daily until platelet count and LDH normalize
Removes autoantibodies and replenishes ADAMTS-13
Adjuncts:
Glucocorticoids (e.g. prednisolone or methylprednisolone)
Rituximab (anti-CD20) in relapsing or refractory cases
Caplacizumab:
Monoclonal antibody that blocks vWF–platelet interaction
Shortens time to response, reduces recurrence
– Platelet transfusion is contraindicated unless life-threatening bleeding occurs.
Differential Diagnosis
HUS (haemolytic uraemic syndrome) – more renal, less neuro
DIC – ↑ PT/APTT, ↓ fibrinogen, ↑ D-dimer
Sepsis-related MAHA
Malignant hypertension
HELLP syndrome (pregnancy)
Complications
Stroke
Renal failure
Cardiac involvement
Relapse (seen in up to 40%)
Death if untreated (mortality ~90%); with treatment ~10–20%
Prognosis
Good with early plasma exchange
Long-term follow-up needed for relapse or chronic ADAMTS-13 deficiency
Monitor platelet count, LDH, and ADAMTS-13 activity