1- Definition and Classification
2-Epidemiology
3-Pathophysiology
4- Clinical Features
5– Investigations
6- Autoantibodies
7- Malignancy Screening
8- Pulmonary Involvement
9- Management Overview
10- Juvenile Dermatomyositis (JDM)
11- Differential Diagnoses
Polymyositis (PM) and Dermatomyositis (DM) are autoimmune myopathies characterised by:
Symmetrical proximal muscle weakness
Elevated muscle enzymes (e.g. CK)
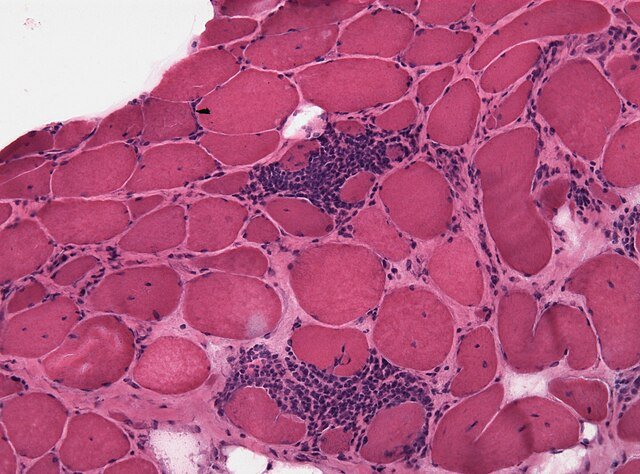
Inflammatory muscle biopsy
Dermatomyositis also features:
Distinctive skin manifestations (e.g. heliotrope rash, Gottron’s papules)
Perivascular and perifascicular inflammation on biopsy
-DM is considered complement-mediated microangiopathy, while PM reflects direct T-cell cytotoxicity
Rare: ~2–10 per million/year
Age of onset: 40–60 years
Female predominance
Juvenile form: Juvenile dermatomyositis (JDM)—onset before age 18
Immune-mediated muscle fibre destruction
PM: CD8+ T cells invade muscle fibres
DM: CD4+ T cells, complement, and perivascular inflammation
Triggered by infections, malignancy, or drugs in some cases
Symmetrical proximal muscle weakness
Difficulty climbing stairs, standing up, lifting arms
Muscle pain in 1/3 of cases
Dysphagia (pharyngeal weakness) in severe cases
Fatigue, weight loss
Heliotrope rash: violaceous rash around eyelids
Gottron’s papules: scaly papules over knuckles
Shawl sign, V-sign: erythema over chest, neck
Mechanic’s hands: rough, cracked skin on fingers
–Skin signs may precede, accompany, or follow muscle symptoms

| Test | Findings |
|---|---|
| CK, AST, LDH | Raised (due to muscle damage) |
| ANA | Positive in 30–80% of cases |
| Myositis-specific antibodies | e.g. Anti-Jo-1 (esp. with ILD) |
| EMG | Myopathic pattern: short-duration, polyphasic potentials |
| MRI | Shows inflamed muscles—guides biopsy site |
| Muscle biopsy | Diagnostic: endomysial (PM) vs. perivascular (DM) inflammation |
| Autoantibody | Associated Features |
|---|---|
| Anti-Jo-1 | Myositis + ILD + arthritis (“antisynthetase syndrome”) |
| Anti-Mi-2 | Classic DM rash |
| Anti-SRP | Severe PM |
| ANA | Often positive (nonspecific) |
Dermatomyositis is a paraneoplastic condition in many adults
Search for underlying cancer (esp. lung, ovarian, breast, GI):
CT chest/abdomen/pelvis, mammography, PSA, GI endoscopy
PM less strongly associated but still warrants evaluation
Seen especially in anti-Jo-1–positive patients
Interstitial lung disease (ILD) is common
Can cause exertional dyspnoea, dry cough
Pulmonary fibrosis may worsen prognosis
| Step | Treatment |
|---|---|
| Induction | Prednisolone 1 mg/kg/day ± IV methylpred (for severe cases) |
| Steroid-sparing agents | Methotrexate, Azathioprine, MMF |
| Refractory disease | IVIg, cyclophosphamide (if ILD or severe skin), rituximab (limited evidence) |
| Skin disease | May benefit from hydroxychloroquine (especially in DM) |
| Supportive | Physiotherapy, calcium/vitamin D, screen for osteoporosis |
Peak onset ~7 years
Often monophasic or relapsing-remitting
Calcinosis cutis and skin ulceration are more common
Same core treatments: steroids + MTX ± IVIg
Inclusion body myositis: older adults, distal > proximal weakness, poor steroid response
Drug-induced myopathy: statins, steroids
Hypothyroidism
Muscular dystrophies (especially if young onset)