Actinic Keratosis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Investigations & Lab Results
5- Complications
6- Treatment
Introduction
Actinic keratosis , also known as solar keratosis, is a common precancerous skin condition that arises due to prolonged exposure to ultraviolet (UV) radiation from the sun. It manifests as rough, scaly, or crusty patches typically found on sun-exposed areas such as the face, ears, scalp, neck, and hands. These lesions result from abnormal growth of keratinocytes in the epidermis caused by cumulative UV damage. Actinic keratosis is most frequently seen in fair-skinned, older adults who have had significant lifetime sun exposure. Although AK itself is not invasive cancer, it is considered an early warning sign because it can potentially progress to squamous cell carcinoma, a type of skin cancer.

Causes
Chronic and cumulative exposure to ultraviolet (UV) radiation, especially UVB rays from sunlight
Fair skin that burns easily and tans poorly
Older age with longer lifetime sun exposure
History of frequent or severe sunburns
Living in regions with high sun intensity or at high altitudes
Immunosuppression, such as in organ transplant recipients or people with HIV/AIDS
Exposure to artificial UV sources, like tanning beds
Genetic susceptibility and skin type also play a role in risk development
Symptoms
Rough, dry, or scaly patch on sun-exposed skin
Usually small (1–2 cm), but may be larger
Color varies: pink, red, brown, or skin-colored
Often feels like sandpaper or rough to touch
May be flat or slightly raised
Sometimes itchy or tender, but often asymptomatic
Lesions commonly appear on the face, ears, scalp, neck, forearms, and backs of the hands
Can develop as a single lesion or multiple lesions clustered together
Investigations & Lab Results
1. Clinical Diagnosis
Actinic keratosis is primarily diagnosed based on clinical examination of the characteristic skin lesions on sun-exposed areas.
Diagnosis is often straightforward due to the typical appearance and history of sun exposure.
2. Dermoscopy
A non-invasive tool used to examine skin lesions more closely.
Features supporting AK diagnosis include:
Erythematous background
Scaly surface
Woolly or ropy white structures
Hairpin vessels
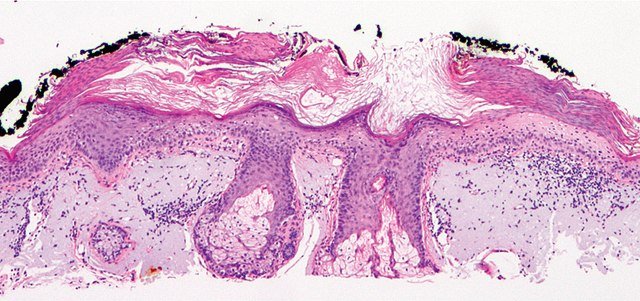
3. Skin Biopsy
Performed if the diagnosis is uncertain or if there is suspicion of progression to squamous cell carcinoma (SCC).
Histopathology shows:
Atypical keratinocytes confined to the basal and suprabasal layers of the epidermis
Parakeratosis (retention of nuclei in the stratum corneum)
Solar elastosis (damage to dermal collagen due to UV radiation)
No invasion into the dermis (distinguishes AK from SCC)
4. Other Tests
Usually not required, but may include photographic documentation for monitoring lesion changes over time.
Complications
Progression to Squamous Cell Carcinoma (SCC):
The most significant complication is the potential for AK lesions to develop into invasive squamous cell carcinoma, a type of skin cancer. Not all AKs progress, but the risk exists, especially with untreated or multiple lesions.
Local Skin Damage:
Persistent lesions can cause chronic irritation, redness, scaling, and sometimes tenderness or bleeding.
Cosmetic Concerns:
Lesions may cause visible scaly patches or crusts on exposed skin, leading to cosmetic disfigurement.
Field Cancerization:
The surrounding skin may also be damaged by UV exposure, harboring multiple subclinical lesions, increasing the risk of widespread skin cancer development.
Recurrence:
Even after treatment, AKs can recur, necessitating ongoing monitoring and sun protection.
Treatment
1. Topical Treatments
-
5-Fluorouracil (5-FU):
-
A chemotherapy cream that destroys abnormal skin cells.
-
Applied for several weeks; causes redness, irritation, and crusting.
-
-
Imiquimod:
-
An immune response modifier that stimulates the body’s immune system to attack abnormal cells.
-
Applied several times per week over weeks.
-
-
Diclofenac gel:
-
A nonsteroidal anti-inflammatory agent used for mild lesions.
-
Less irritating but slower acting.
-
-
Ingenol mebutate:
-
Causes rapid destruction of abnormal cells with a short treatment course.
-
2. Procedural Treatments
-
Cryotherapy:
-
Freezing lesions with liquid nitrogen; common, quick, and effective.
-
Causes blistering and crusting that heals over days to weeks.
-
-
Curettage and Electrosurgery:
-
Scraping off the lesion followed by cauterization.
-
-
Photodynamic Therapy (PDT):
-
Application of a photosensitizing agent followed by exposure to a specific light source, destroying abnormal cells.
-
Useful for multiple or large lesions.
-
-
Laser Therapy:
-
Ablative lasers can remove lesions, often reserved for resistant cases.
-
3. Preventive Measures
-
Sun protection:
-
Use of broad-spectrum sunscreens, protective clothing, and avoidance of peak sun hours.
-
Critical to prevent new lesions and recurrence.
-
-
Regular skin examinations:
-
For early detection of new or recurrent lesions.
-