Candidiasis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Types of Candidiasis
5- Complications
6- Treatment
Introduction
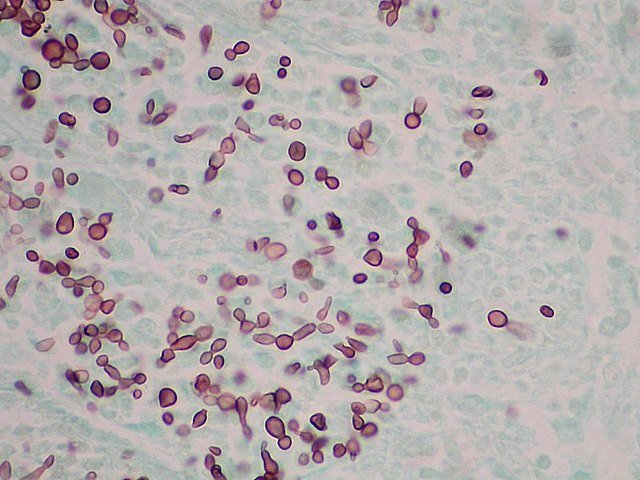
Candidiasis is a fungal infection caused by yeasts of the genus Candida, most commonly Candida albicans. These fungi are part of the normal flora of the skin, mouth, gastrointestinal tract, and vagina but can become opportunistic pathogens under certain conditions, leading to infection.
Candidiasis can range from superficial (e.g., oral thrush, vaginal yeast infection, intertrigo) to invasive/systemic disease, particularly in immunocompromised individuals such as those with HIV/AIDS, cancer, diabetes, or those on prolonged antibiotics or corticosteroids.
The infection occurs when there’s a disruption in the normal microbial balance or weakened host defenses, allowing Candida to overgrow. Candidiasis may present as localized mucocutaneous infection or, in severe cases, as disseminated candidiasis involving the bloodstream (candidemia), kidneys, liver, and other organs.

Causes
Immunosuppression
HIV/AIDS
Cancer chemotherapy
Organ transplant recipients (on immunosuppressive drugs)
Use of corticosteroids
Antibiotic Use
Broad-spectrum antibiotics disrupt the normal bacterial flora, allowing Candida to overgrow
Diabetes Mellitus
High blood sugar promotes fungal growth
Impaired immune response in diabetic patients
Hormonal Changes
Pregnancy
Use of oral contraceptive pills
Hormone replacement therapy
Moisture and Occlusion
Poorly ventilated skin folds (e.g., under breasts, groin)
Wearing tight or damp clothing
Diaper use in infants
Poor Oral Hygiene / Denture Use
Especially in elderly or debilitated individuals
Malnutrition or Iron Deficiency
Affects immune function and mucosal integrity
Hospitalization / Medical Devices
Central venous catheters
Urinary catheters
Mechanical ventilation
Total parenteral nutrition (TPN)
Neonates and Elderly
Immature or weakened immune systems
Mucosal Injury or Atrophy
Chemotherapy, radiation, or trauma to mucous membranes
Symptoms
1. Oral Candidiasis (Thrush):
White, creamy plaques on the tongue, inner cheeks, gums, or palate
Redness and soreness underneath the plaques
Burning sensation in the mouth
Difficulty swallowing (in more severe or esophageal involvement)
2. Esophageal Candidiasis:
Painful swallowing (odynophagia)
Difficulty swallowing (dysphagia)
Retrosternal chest pain
Often associated with immunosuppression (e.g., HIV/AIDS)
3. Vaginal Candidiasis:
Thick, white, curd-like vaginal discharge
Itching, burning, or irritation of the vulva and vagina
Redness and swelling of the vaginal area
Pain during urination or intercourse
4. Cutaneous Candidiasis (Skin Folds, Diaper Rash, Intertrigo):
Red, moist, macerated rash with satellite pustules or papules
Common in warm, moist areas (e.g., under breasts, groin, axillae, buttocks)
Itching, burning, and discomfort
5. Candidal Onychomycosis (Nails):
Discoloration or thickening of the nail
Nail plate separation from the bed
Swelling and redness of the surrounding skin (paronychia)
6. Invasive/Systemic Candidiasis (Candidemia):
Fever and chills not responding to antibiotics
Hypotension, organ dysfunction (in severe sepsis)
May involve the kidneys, liver, eyes (endophthalmitis), brain, heart (endocarditis), and bones
Common in hospitalized or immunocompromised patients with central lines
Types of Candidiasis
1. Oral Candidiasis (Thrush)
Infection of the mucous membranes of the mouth and throat
Common in infants, elderly, and immunocompromised individuals
Includes pseudomembranous, erythematous, and chronic hyperplastic types
2. Esophageal Candidiasis
Infection of the esophagus
Often seen in immunosuppressed patients (e.g., HIV/AIDS)
Causes painful swallowing and chest discomfort
3. Vaginal Candidiasis (Vaginal Yeast Infection)
Infection of the vulva and vagina
Common in women of reproductive age
Causes itching, discharge, and irritation
4. Cutaneous Candidiasis
Infection of the skin, especially in warm, moist areas (intertrigo)
Also includes diaper rash in infants and candidal paronychia (around nails)
5. Candidal Onychomycosis
Fungal infection of the nails
Causes thickened, brittle, discolored nails
6. Invasive or Systemic Candidiasis
Occurs when Candida enters the bloodstream (candidemia)
Can spread to organs such as kidneys, liver, eyes, heart, and brain
Common in hospitalized, immunocompromised, or critically ill patients
7. Chronic Mucocutaneous Candidiasis
Persistent or recurrent candidiasis involving skin, nails, and mucous membranes
Often due to underlying immune defects
Complications
Disseminated (Invasive) Candidiasis
Spread of Candida into the bloodstream (candidemia) and multiple organs
Can cause sepsis, organ failure, and death if untreated
Common sites affected include kidneys, liver, spleen, eyes (endophthalmitis), heart (endocarditis), bones, and brain
Chronic Mucocutaneous Candidiasis
Persistent or recurrent infection of skin, nails, and mucous membranes due to immune dysfunction
May cause scarring and disfigurement
Esophageal Stricture
From repeated or severe esophageal candidiasis leading to narrowing of the esophagus and swallowing difficulties
Secondary Bacterial Infection
Superimposed bacterial infection of the affected mucosa or skin due to breakdown of natural barriers
Oral Candidiasis-Related Nutritional Problems
Pain and difficulty swallowing may lead to poor oral intake and weight loss
Nail Deformity
Chronic nail infections can cause permanent changes in nail shape and function
Psychosocial Impact
Chronic or visible candidiasis (e.g., oral thrush, diaper rash) can cause distress or social embarrassment
Treatment
1. Topical Antifungal Therapy
Used for mild, localized mucocutaneous infections:
Oral candidiasis (mild):
Nystatin suspension or lozenges
Clotrimazole troches
Miconazole gel
Vaginal candidiasis:
Clotrimazole or miconazole creams or suppositories
Nystatin vaginal tablets
Cutaneous candidiasis:
Clotrimazole, miconazole, or ketoconazole creams
Keep affected areas dry and clean
2. Systemic Antifungal Therapy
Required for moderate to severe infections, esophageal candidiasis, invasive disease, or immunocompromised patients:
Fluconazole:
First-line oral agent for most candidiasis types
Dose and duration depend on infection site and severity
Itraconazole:
Alternative to fluconazole, especially in refractory cases
Amphotericin B:
Used for severe systemic infections or fluconazole-resistant strains
Usually given intravenously
Echinocandins (Caspofungin, Micafungin, Anidulafungin):
Used for invasive candidiasis, especially in hospitalized patients
Intravenous administration
Posaconazole and Voriconazole:
Used in resistant or complicated cases
3. Supportive Measures
Control predisposing factors (e.g., diabetes, antibiotic use)
Maintain good hygiene and dryness of affected areas
Proper denture care for oral candidiasis
Avoid irritants and tight clothing in cutaneous infections
4. Special Situations
Neonates: Use nystatin or fluconazole carefully under pediatric guidance
Recurrent vaginal candidiasis: Consider longer antifungal courses and investigate underlying causes
Immunocompromised patients: Often require prolonged systemic therapy and monitoring