Kaposi Sarcoma
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Types of Kaposi Sarcoma
5- Investigations & Lab Results
6- Complications
7- Treatment
Introduction
Kaposi Sarcoma (KS) is a malignant tumor that arises from endothelial cells lining blood or lymphatic vessels. It is strongly associated with infection by Human Herpesvirus 8 (HHV-8), also known as Kaposi Sarcoma-associated herpesvirus (KSHV).
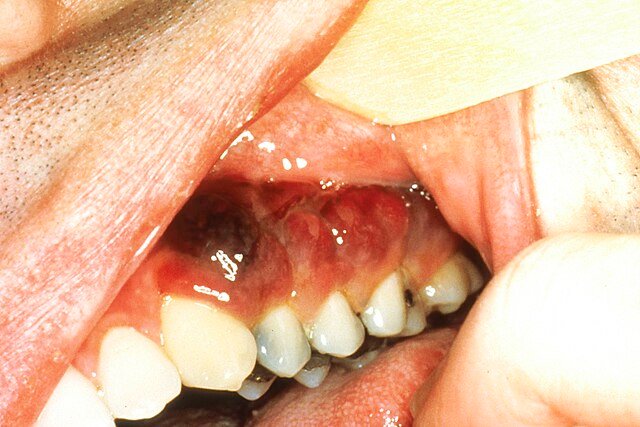
KS is characterized by the development of vascular tumors that appear as purple, red, or brown patches, plaques, or nodules on the skin, but can also involve mucous membranes, lymph nodes, and internal organs (e.g., lungs and gastrointestinal tract).

Causes
HHV-8 Infection (KSHV):
Necessary cause of all forms of KS
Transmitted through saliva, sexual contact, blood transfusion, and organ transplantation
Virus infects endothelial cells and promotes uncontrolled proliferation and angiogenesis
Immunosuppression:
Reduces immune surveillance, allowing HHV-8–infected cells to proliferate
Common in:
HIV/AIDS (especially with low CD4 count)
Organ transplant recipients (due to immunosuppressive therapy)
Cancer patients on chemotherapy
Genetic and Environmental Factors:
May contribute in endemic and classic forms
Higher prevalence in specific geographic areas (e.g., sub-Saharan Africa, Mediterranean regions)
Male Gender:
KS is more common in males across all subtypes, though the reasons are not fully understood
Symptoms
1. Skin Lesions (Most Common Symptom)
Color: Pink, red, purple, brown, or dark blue
Shape: Macules (flat), papules, plaques, or nodules
Texture: May be smooth, raised, or firm
Location: Face, legs (especially lower limbs), feet, genital area, and oral mucosa
Pattern: May occur singly or in clusters, often symmetric
Progression: Lesions may enlarge, coalesce, or ulcerate
2. Mucous Membrane Involvement
Lesions on the oral cavity (especially hard palate, gums, or tongue)
May cause discomfort, bleeding, or difficulty eating
3. Lymph Node Involvement
Painless swelling of lymph nodes
Can cause lymphedema (swelling of limbs or face due to lymphatic obstruction)
4. Visceral Involvement (Internal Organs)
Seen mostly in AIDS-associated or immunosuppressed patients:
Gastrointestinal tract:
Abdominal pain, bleeding, weight loss, or diarrhea
May be asymptomatic or detected incidentally
Lungs (Pulmonary KS):
Shortness of breath, cough, chest pain, or hemoptysis
Can be life-threatening
5. Constitutional Symptoms (in advanced disease)
Fever
Night sweats
Weight loss
Fatigue
Types of Kaposi Sarcoma
1. Classic Kaposi Sarcoma
Population: Elderly men of Mediterranean, Eastern European, or Middle Eastern origin
Course: Slow-growing and indolent
Lesions: Purple to dark brown skin nodules, mainly on the lower legs and feet
Systemic involvement: Rare
Prognosis: Generally good; often doesn’t require aggressive treatment
2. Endemic (African) Kaposi Sarcoma
Geography: Sub-Saharan Africa
Population: Affects both adults and children (particularly prepubertal boys)
Course: More aggressive than classic KS
Lesions: Extensive skin involvement; may affect lymph nodes and internal organs
Prognosis: Variable; can be life-threatening, especially in children
3. Iatrogenic (Immunosuppression-associated) Kaposi Sarcoma
Population: Organ transplant recipients or patients on long-term immunosuppressive therapy
Trigger: Immunosuppressive medications (e.g., corticosteroids, cyclosporine)
Lesions: Skin and mucosal lesions; may involve viscera
Prognosis: May regress with reduction of immunosuppressive therapy
4. AIDS-related (Epidemic) Kaposi Sarcoma
Population: People living with HIV/AIDS (especially with CD4 counts <200 cells/µL)
Course: Aggressive, rapidly progressive
Lesions: Widespread skin, mucosal, lymph node, and visceral involvement (lungs, GI tract)
Prognosis: Depends on response to antiretroviral therapy (ART) and extent of disease
Treatment: Often requires both ART and chemotherapy
Investigations & Lab Results
1. Clinical Examination
Careful inspection of skin, oral mucosa, and genital areas for characteristic lesions
Palpation for lymphadenopathy or limb swelling (lymphedema)
2. Skin or Lesion Biopsy
Gold standard for diagnosis
Histopathological findings:
Spindle-shaped cells forming vascular slits
Extravasated red blood cells
Hemosiderin deposition
Infiltration with inflammatory cells
Immunohistochemistry: Positive for HHV-8 (LANA-1 antigen) in tumor cells
3. Laboratory Tests
HIV testing: All patients with suspected KS should be tested for HIV
CD4 count and HIV viral load:
CD4 count <200 cells/µL common in AIDS-related KS
Complete Blood Count (CBC):
May show anemia or cytopenias in advanced disease
Liver and renal function tests: Baseline before systemic therapy
4. Imaging Studies (to assess visceral involvement)
Chest X-ray or CT scan: Evaluate for pulmonary KS (e.g., nodular infiltrates, pleural effusions)
Abdominal ultrasound or CT scan: Check for involvement of liver, spleen, or lymph nodes
Endoscopy or colonoscopy: For GI symptoms or suspected GI KS (may reveal submucosal nodules or bleeding)
5. Other Investigations (as needed)
Bronchoscopy: If pulmonary KS is suspected
Lymph node biopsy: If lymphadenopathy is present
PCR testing for HHV-8 DNA: Rarely used but available in research or complex cases
Complications
1. Skin and Mucosal Complications
Ulceration and secondary infection of lesions
Bleeding, especially from oral or mucosal lesions
Disfigurement and psychosocial distress
Lymphedema due to lymphatic obstruction, often in the legs, genital area, or face
Functional impairment, especially if lesions involve eyelids, hands, or joints
2. Pulmonary Involvement
Can cause life-threatening respiratory compromise
Symptoms: cough, shortness of breath, hemoptysis, chest pain
Pleural effusions may develop, leading to breathing difficulty
May resemble pneumonia or tuberculosis on imaging
3. Gastrointestinal Involvement
Bleeding: May cause melena or hematemesis
Obstruction or pain: If large or numerous lesions are present
Often asymptomatic, but complications may emerge with progression
4. Lymphatic and Systemic Involvement
Generalized lymphadenopathy
Severe lymphedema causing chronic swelling and secondary infections
Cachexia, fever, night sweats, and weight loss in advanced disease
5. Treatment-Related Complications
Chemotherapy toxicity: Myelosuppression, fatigue, nausea
Drug interactions with ART or immunosuppressants
Immune reconstitution inflammatory syndrome (IRIS): Worsening of KS after starting ART due to recovering immune response
6. Mortality
Death may occur due to complications of visceral involvement, particularly pulmonary or gastrointestinal KS, or due to opportunistic infections in immunocompromised patients.
Treatment
Antiretroviral Therapy (ART) – For AIDS-related KS
First-line treatment in HIV-positive patients
ART alone can lead to regression of KS lesions in early or mild cases
May be combined with chemotherapy for extensive or rapidly progressing disease
2. Local Treatments – For limited skin or mucosal disease
Cryotherapy: Freezing of superficial lesions
Surgical excision: For isolated or cosmetically bothersome lesions
Radiation therapy: Effective for localized lesions, particularly in classic or endemic KS
Topical agents:
Alitretinoin gel (0.1%) – for cutaneous lesions
Imiquimod cream – immune response modifier (limited efficacy)
3. Systemic Chemotherapy – For advanced, symptomatic, or visceral disease
Indicated for:
Rapidly progressing KS
Extensive skin involvement
Pulmonary, gastrointestinal, or lymphatic KS
Poor response to ART alone
Common regimens:
Liposomal doxorubicin (preferred due to lower toxicity)
Paclitaxel (for refractory or aggressive cases)
Vincristine, bleomycin, or etoposide (used in some settings)
4. Immunomodulatory and Targeted Therapies (in specific or refractory cases)
Interferon-alpha: For early-stage disease with good immune function (less used now)
Immune checkpoint inhibitors (e.g., nivolumab): Under investigation for advanced or recurrent KS
Thalidomide or lenalidomide: Occasionally used in difficult-to-treat cases
5. Management of Iatrogenic KS (post-transplant)
Reduce or adjust immunosuppressive therapy when possible
Switch to mTOR inhibitors (e.g., sirolimus), which may help control KS while maintaining graft function