Keloids / Hypertrophic Scars
Content of This Page
1- Definition & Distinction
2-Aetiology & Risk Factors
3-Pathophysiology
4- Clinical Presentation
5- Histological Differences
6- Differential Diagnosis
7- Treatment Strategies
8- Prevention & Patient Education
9- Core Summary Points
Definition & Distinction
Hypertrophic scars are raised, red scars that stay within the boundaries of the original wound.
Keloids are raised, firm scars that grow beyond the original wound margins and do not regress spontaneously.
| Feature | Hypertrophic Scar | Keloid |
|---|---|---|
| Definition | Thickened scar that remains within the boundary of original wound | Scar that extends beyond the original wound margins |
| Growth pattern | Stabilizes or regresses over time | May continue growing for months/years |
| Histology | Collagen in parallel bundles | Thick, haphazard collagen bundles (type I & III) |

Aetiology & Risk Factors
Skin trauma: surgery, burns, piercings, tattoos, acne
Genetic predisposition: more common in individuals of African, Asian, or Hispanic descent
Younger age: more common in ages 10–30
High-tension areas: chest, shoulders, upper back, earlobes
Pathophysiology
Abnormal wound healing response involving:
↑ fibroblast activity
Excess collagen synthesis (mainly Type I and III)
↓ collagen degradation (due to low collagenase)
↑ growth factors (e.g. TGF-β)
Keloids: have a persistent proliferative and inflammatory response
Clinical Presentation
| Feature | Hypertrophic Scar | Keloid |
|---|---|---|
| Location | At wound site | Extends beyond |
| Onset | Weeks after injury | Months after injury |
| Symptoms | May be itchy/painful | Often painful, pruritic |
| Progression | May regress over time | Often progressive |
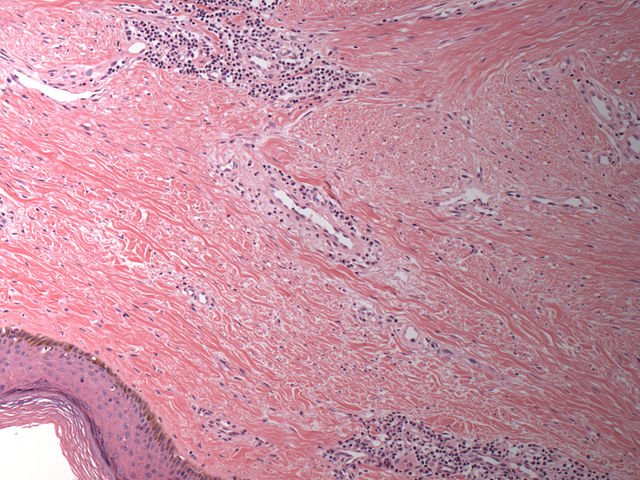
Histological Differences
Hypertrophic scar:
Collagen arranged in parallel bundles
More confined vascularity
Keloid:
Thick, haphazard collagen bundles
Prominent blood vessels, chronic inflammation
Differential Diagnosis
Dermatofibroma
Dermatofibrosarcoma protuberans (DFSP)
Hypertrophic lupus lesions
Scleroderma plaques
Biopsy may be required if diagnosis is uncertain or malignancy is suspected.
Treatment Strategies
First-line:
Intralesional corticosteroids (e.g. triamcinolone)
Reduces inflammation and collagen production
– Adjuncts:
Silicone gel sheeting or dressings
Compression therapy (earrings, pressure garments)
Topical imiquimod (for post-excision keloid prevention)
– Advanced Options:
5-fluorouracil (5-FU) or bleomycin injections
Pulsed dye laser therapy
Cryotherapy (esp. for smaller keloids)
– Surgical Excision:
Only in combination with steroids, radiotherapy, or silicone to prevent recurrence
Prevention & Patient Education
Avoid unnecessary cosmetic procedures in high-risk patients
Use sterile techniques in piercings or surgeries
Apply silicone gel sheets after wounds or surgery
Educate patients on early treatment signs of raised scarring
Core Summary Points
Keloid = outgrows wound boundary, recurs frequently
Hypertrophic scar = raised but remains within wound, may regress
Corticosteroids are the first-line treatment
Always use multimodal therapy for resistant cases
Prevention is better than cure—especially in high-risk ethnic groups