Psoriasis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of Disease
5- Treatment
6- What Should You Avoid
Introduction
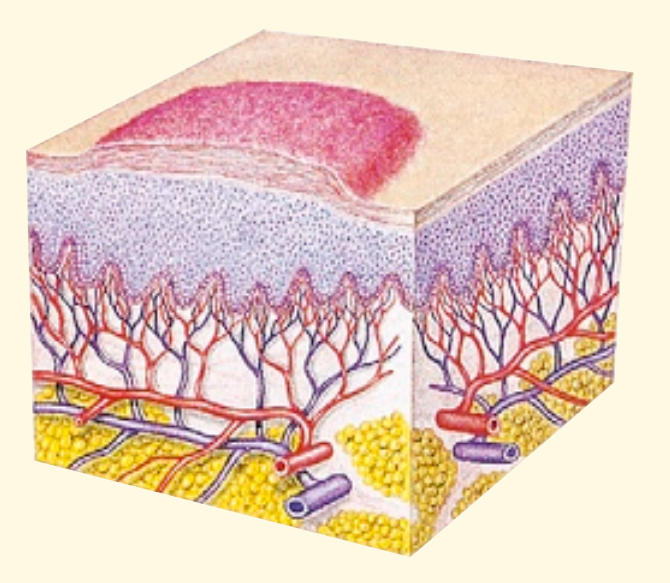
Psoriasis is a chronic autoimmune skin condition that speeds up the life cycle of skin cells, causing them to build up rapidly on the surface of the skin. This buildup of cells leads to scaling on the skin’s surface. Inflammation and redness around the scales are also common. Psoriasis typically occurs on the elbows, knees, scalp, and lower back, but it can appear anywhere on the body.
Causes
The exact cause of psoriasis is not fully understood, but it is believed to involve an immune system issue related to T cells and other white blood cells. Genetics also play a role, as psoriasis tends to run in families.
Triggers:
Certain factors can trigger or exacerbate psoriasis, including:
- Stress
- Skin injuries (cuts, scrapes, sunburn)
- Infections (such as strep throat)
- Certain medications
- Cold, dry weather
- Heavy alcohol consumption
- Smoking
Symptoms
- Red patches of skin covered with thick, silvery scales
- Dry, cracked skin that may bleed
- Itching, burning, or soreness
- Thickened or pitted nails
- Swollen and stiff joints (in psoriatic arthritis)

Stages of Disease
1. Mild Psoriasis
- Symptoms: In mild cases, psoriasis affects less than 3% of the body. The plaques are usually small and localized. They may cause some discomfort but generally do not interfere significantly with daily life.
- Appearance: Small, red patches with silvery scales, often on the elbows, knees, scalp, or lower back.
2. Moderate Psoriasis
- Symptoms: Moderate psoriasis covers 3-10% of the body surface. The plaques are more widespread and may cause more significant discomfort, including itching and burning.
- Appearance: Larger plaques that may be more numerous, affecting more areas such as the scalp, nails, and other body parts.
3. Severe Psoriasis
Symptoms: Severe psoriasis affects more than 10% of the body surface area. It can significantly impact the quality of life, causing physical discomfort and emotional distress. Psoriatic arthritis may also develop in some individuals.
Appearance: Extensive areas of red, inflamed skin covered with thick, silvery scales. The plaques can merge into large areas of affected skin.
Treatment
While there is no cure for psoriasis, treatments can help manage symptoms. These include:
Topical Treatments: Creams and ointments, such as corticosteroids, vitamin D analogs, and retinoids.
Phototherapy: Controlled exposure to ultraviolet light.
Systemic Medications: Oral or injected medications that affect the entire body, including biologics that target specific parts of the immune system.
Lifestyle Changes: Managing stress, maintaining a healthy diet, and avoiding triggers.
What Should You Avoid
1. Stress
- Impact: Stress is a well-known trigger for psoriasis flare-ups. The body’s stress response can lead to inflammation, exacerbating symptoms.
- Management: Practice stress-reducing activities like yoga, meditation, deep breathing exercises, or spending time on hobbies.
2. Skin Injuries
- Impact: Injuries to the skin, such as cuts, scrapes, insect bites, or even sunburn, can trigger a psoriasis flare-up, a phenomenon known as the Koebner response.
- Management: Protect your skin by being cautious when shaving, using sunscreen, and avoiding activities that could lead to skin trauma.
3. Certain Medications
- Impact: Some medications can trigger or worsen psoriasis. These include:
- Beta-blockers (used for high blood pressure)
- Lithium (used for bipolar disorder)
- Antimalarials
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- Management: Always inform your healthcare provider about your psoriasis when being prescribed new medications.
4. Alcohol
- Impact: Heavy alcohol consumption can interfere with the effectiveness of psoriasis treatments and may trigger flare-ups.
- Management: Limit or avoid alcohol to help manage symptoms and improve treatment outcomes.
5. Smoking
- Impact: Smoking is a significant risk factor for both developing psoriasis and worsening existing symptoms. It can also decrease the effectiveness of treatments.
- Management: Quitting smoking can help reduce the severity of psoriasis and improve overall health.
6. Cold, Dry Weather
- Impact: Cold weather can dry out the skin, leading to increased itching, scaling, and discomfort.
- Management: Use a humidifier indoors, apply moisturizers regularly, and protect your skin from the cold by wearing appropriate clothing.
7. Certain Foods
- Impact: While there is no specific “psoriasis diet,” some people find that certain foods can trigger flare-ups. Common culprits include:
- Red meat and processed foods
- Dairy products
- Gluten (in those who are sensitive)
- Sugary foods and beverages
- Management: Keep a food diary to identify any foods that may trigger your symptoms and discuss dietary changes with your healthcare provider.
8. Infections
- Impact: Infections, particularly streptococcal throat infections, can trigger or worsen psoriasis, especially in children and young adults.
- Management: Practice good hygiene, seek prompt treatment for infections, and consider vaccines to reduce the risk of illness.
9. Harsh Skin Care Products
- Impact: Certain soaps, detergents, and skin care products can irritate the skin, potentially leading to flare-ups.
- Management: Choose gentle, fragrance-free products, and avoid using harsh scrubs or exfoliants on affected areas.
10. Excessive Sun Exposure
- Impact: While moderate sunlight can help improve psoriasis symptoms, too much sun can cause sunburn, leading to a flare-up.
- Management: Spend time in the sun gradually, use sunscreen on unaffected areas, and avoid getting sunburned.
11. Obesity
- Impact: Excess weight can exacerbate psoriasis symptoms and increase the risk of developing psoriatic arthritis.
- Management: Maintaining a healthy weight through a balanced diet and regular exercise can help manage symptoms.