Stevens-Johnson Syndrome (SJS)
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Investigations & Lab Results
5- Drugs Associated With Stevens-Johnson Syndrome
6- Complications
7- Treatment
Introduction
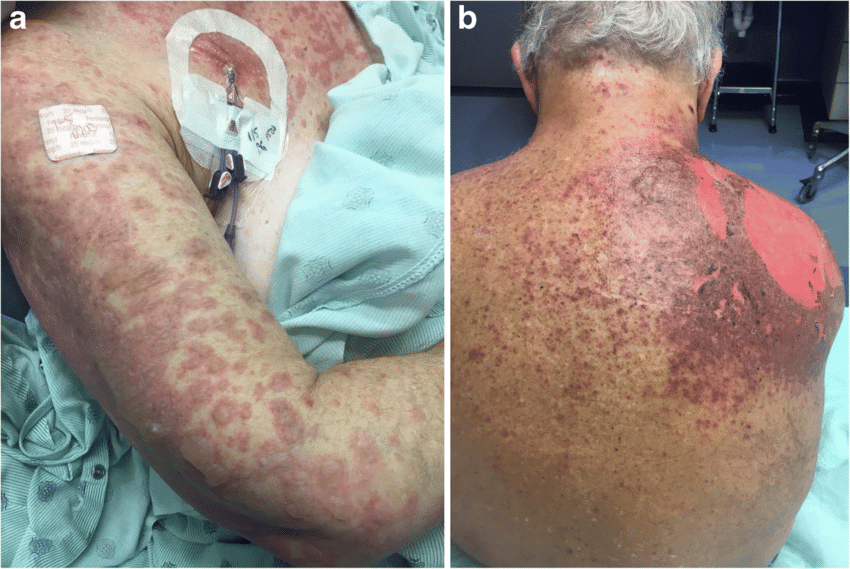
Stevens-Johnson Syndrome (SJS) is a rare but serious and potentially life-threatening disorder characterized by a severe hypersensitivity reaction that affects the skin and mucous membranes. It usually presents as widespread painful rash, blisters, and peeling of the skin, along with involvement of mucosal surfaces such as the mouth, eyes, and genitals. SJS is most often triggered by adverse reactions to medications, infections, or, rarely, other factors. Because it causes extensive skin damage similar to a severe burn, prompt recognition and treatment are critical to reduce complications and improve outcomes.
Causes
Medications (most common cause):
Antibiotics (e.g., sulfonamides, penicillins, cephalosporins)
Anticonvulsants (e.g., phenytoin, carbamazepine, lamotrigine)
Nonsteroidal anti-inflammatory drugs (NSAIDs)
Allopurinol
Antiretroviral drugs
Infections:
Mycoplasma pneumoniae
Herpes simplex virus
Other viral infections (e.g., HIV, influenza)
Bacterial infections
Idiopathic:
In some cases, no clear cause is identified.
Other triggers:
Vaccinations (rare)
Malignancies (rare association)

Symptoms
Initial symptoms (prodromal phase):
Fever
Malaise, fatigue
Sore throat
Cough
Headache
Skin and mucous membrane involvement:
Painful red or purplish rash that spreads rapidly
Blisters and target-like (bull’s-eye) lesions on the skin
Widespread skin peeling and sloughing (epidermal detachment)
Mucosal erosions and ulcers affecting the mouth, eyes, lips, genitalia, and sometimes the respiratory or gastrointestinal tract
Other symptoms:
Difficulty swallowing or eating due to painful oral ulcers
Eye redness, pain, swelling, and possible vision problems
Painful urination or genital discomfort
Investigations & Lab Results
1. Clinical Diagnosis
Diagnosis is primarily clinical, based on the characteristic skin and mucosal findings along with history of drug exposure or infection.
2. Laboratory Tests
Complete blood count (CBC):
May show leukopenia or leukocytosis, anemia
Elevated inflammatory markers (ESR, CRP)
Liver and renal function tests:
To assess organ involvement or drug toxicity
Electrolytes:
To monitor dehydration and electrolyte imbalances from skin loss and mucosal involvement
Coagulation profile:
To check for bleeding tendencies or DIC (disseminated intravascular coagulation)
3. Microbiological Studies
Blood cultures and wound cultures:
To identify secondary infections and guide antibiotic therapy
Tests for underlying infections:
Mycoplasma pneumoniae serology or PCR
Viral cultures or PCR if herpes simplex or other viruses suspected
4. Skin Biopsy
Confirms diagnosis by showing:
Full-thickness epidermal necrosis
Subepidermal blister formation
Minimal inflammation in the dermis
5. Other Tests
Chest X-ray:
To assess for respiratory complications if symptoms present
Drugs Associated With Stevens-Johnson Syndrome
1. Antibiotics
-
Sulfonamides (e.g., sulfamethoxazole-trimethoprim) – most frequently implicated
-
Penicillins
-
Cephalosporins
-
Quinolones (e.g., ciprofloxacin)
2. Anticonvulsants (antiepileptics)
-
Phenytoin
-
Carbamazepine
-
Lamotrigine
-
Phenobarbital
-
Valproic acid (less common)
3. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs)
-
Especially oxicam derivatives (e.g., piroxicam, meloxicam)
-
Ibuprofen and naproxen (rare, but reported)
4. Allopurinol
-
A uric acid–lowering agent commonly used in gout
-
High risk, especially in patients with renal impairment
5. Antiretroviral Drugs
-
Nevirapine
-
Abacavir (hypersensitivity reaction)
6. Others
-
Methotrexate
-
Dapsone
-
Modafinil
-
Sertraline and other SSRIs (rarely)
Complications
1. Skin and Mucosal Complications
Secondary skin infections, including cellulitis and sepsis
Scarring, hyperpigmentation, or hypopigmentation
Nail loss or dystrophy
Chronic mucosal damage, such as strictures or adhesions in the eyes, mouth, or genitals
2. Ocular Complications
Conjunctivitis, corneal ulceration, or uveitis
Dry eyes, symblepharon (adhesion of eyelid to eyeball)
Blindness (in severe or untreated cases)
3. Respiratory Complications
Bronchial epithelial sloughing, pneumonia, or acute respiratory distress syndrome (ARDS)
Risk of long-term pulmonary fibrosis
4. Renal and Hepatic Complications
Acute kidney injury
Liver dysfunction or failure, especially if drug-induced
5. Gastrointestinal Complications
Esophageal strictures, erosions, or bleeding
Malnutrition due to oral pain and feeding difficulty
6. Psychosocial and Functional Impact
Chronic pain and fatigue
Psychological trauma, depression, anxiety
Long-term disability due to scarring or vision loss
7. Mortality
SJS carries a mortality rate of around 5–10%, which increases significantly in more severe forms such as Toxic Epidermal Necrolysis (TEN).
Treatment
1. Immediate Measures
Immediate discontinuation of the suspected causative drug
This is the most critical step in halting progression.
2. Supportive Care (Mainstay of Treatment)
Hospitalization in ICU or burn unit
Fluid and electrolyte management to prevent dehydration from skin loss
Nutritional support, possibly with feeding tube if oral ulcers are severe
Pain control with analgesics
Wound care with non-adhesive dressings and aseptic technique
Temperature regulation to compensate for impaired skin barrier
Eye care with lubricants and ophthalmologic consultation
Prevention and treatment of secondary infections, including sepsis monitoring
3. Pharmacologic Treatments (controversial and case-dependent)
Systemic corticosteroids
May be used early in the course but carry a risk of infection; use remains debated.
Intravenous immunoglobulin (IVIG)
Believed to inhibit Fas-mediated apoptosis; used in some cases with variable results.
Cyclosporine
Immunosuppressive drug shown in some studies to reduce mortality.
Plasmapheresis
May be used to remove circulating drug metabolites and immune complexes (rarely used).
TNF-alpha inhibitors (e.g., etanercept)
Emerging treatment, still under investigation.
4. Long-Term Management
Multidisciplinary follow-up (dermatology, ophthalmology, urology, etc.)
Treatment of sequelae such as ocular damage, mucosal scarring, or psychological trauma
Avoidance of triggering drugs in the future
Genetic screening (e.g., HLA-B*1502 in Asians before carbamazepine use)