Tinea Infections
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Types of Tinea Infections
5- Complications
6- Treatment
Introduction
Tinea infections, also known as dermatophytosis, are superficial fungal infections of the skin, hair, or nails caused by a group of fungi known as dermatophytes. These fungi thrive on keratin, a protein found in these tissues. Tinea infections are commonly named based on the part of the body affected, such as tinea capitis (scalp), tinea corporis (body), tinea pedis (feet), and tinea unguium (nails, also called onychomycosis).
Dermatophytes responsible for these infections belong to three genera: Trichophyton, Microsporum, and Epidermophyton. Transmission occurs through direct contact with infected individuals, animals, or contaminated surfaces (fomites), and is favored by warm, moist environments.
Tinea infections are common worldwide and can affect individuals of all ages, though some types are more prevalent in specific age groups or settings (e.g., tinea capitis in children, tinea pedis in athletes). Though usually not serious, they can cause itching, redness, scaling, and discomfort, and may lead to secondary bacterial infections if left untreated.

Causes
Fungal Species (Dermatophytes):
Trichophyton (most common, especially T. rubrum, T. mentagrophytes)
Microsporum (e.g., M. canis)
Epidermophyton (e.g., E. floccosum)
Mode of Transmission:
Human-to-human contact (e.g., shared towels, close physical contact)
Animal-to-human contact (e.g., infected pets like cats and dogs)
Soil-to-human contact (rare; some species are geophilic)
Fomite transmission (contaminated surfaces, clothing, combs, shoes)
Risk Factors That Promote Infection:
Warm, humid environments
Excessive sweating (hyperhidrosis)
Poor hygiene
Wearing tight or occlusive clothing/shoes
Skin maceration or minor trauma
Immunosuppression (e.g., diabetes, HIV, steroid use)
Symptoms
-General Symptoms (common to all types):
Itching (pruritus)
Red, scaly patches
Circular or ring-shaped lesions with raised edges
Central clearing in many cases
Cracking, flaking, or peeling skin
Inflammation or irritation around the edges
-Location-Specific Symptoms:
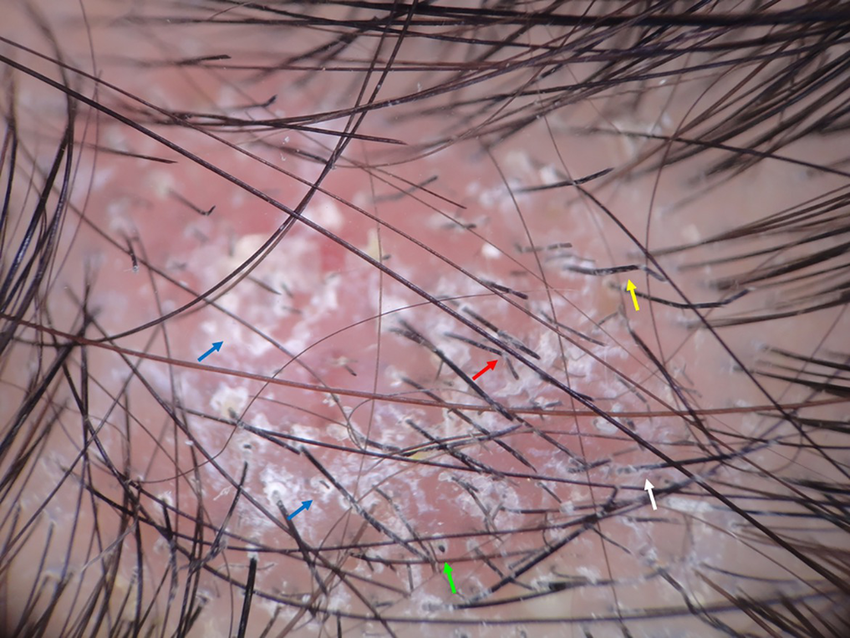
Tinea Capitis (scalp):
Scaly patches on the scalp
Hair loss in affected areas
Black dots from broken hairs
Painful, swollen lesions (kerion in severe cases)
Swollen lymph nodes in the neck
Tinea Corporis (body):
Ring-shaped, red lesions on the trunk or limbs
Clearer center with a red, scaly, and raised border
Itching or mild burning
Tinea Pedis (athlete’s foot):
Itching, burning, or stinging between the toes
Peeling, cracking, or flaking skin
Thickened skin on soles or sides of the feet
Possible blistering
Tinea Cruris (jock itch):
Red, itchy rash in the groin and inner thigh area
Well-defined edges, often with scaling
May be painful or feel like burning
Usually spares the scrotum
Tinea Unguium (onychomycosis – nails):
Thickened, discolored (white, yellow, or brown) nails
Brittle or crumbly texture
Nail distortion or separation from the nail bed
Tinea Barbae (beard area):
Red, inflamed patches in areas with facial hair
Pustules or crusting
Hair loss in the affected area
Pain or swelling in severe infections
Types of Tinea Infections
Tinea Capitis
Affects the scalp and hair shafts
Common in children
Causes scaly patches, hair loss, and sometimes kerion formation
Tinea Corporis
Affects the skin of the trunk and limbs
Presents as ring-shaped lesions with central clearing and raised borders
Also called “ringworm of the body”
Tinea Cruris
Affects the groin, inner thighs, and buttocks
Also called “jock itch”
More common in males, especially in humid climates
Tinea Pedis
Affects the feet, especially between the toes
Also called “athlete’s foot”
Can present as interdigital, moccasin-type, or vesicular form
Tinea Manuum
Affects the palms of the hands
Often seen in individuals with tinea pedis (two feet, one hand syndrome)
Tinea Unguium (Onychomycosis)
Affects the nails (fingernails or toenails)
Causes thickened, discolored, brittle nails
Tinea Barbae
Affects the beard area of the face and neck
Usually occurs in adult men
Can cause pustules, swelling, and hair loss
Tinea Faciei
Affects the non-bearded areas of the face
May resemble tinea corporis but often less scaly and more inflamed
Complications
Secondary Bacterial Infection
Scratching the itchy lesions can break the skin, allowing bacteria (e.g., Staphylococcus aureus) to enter and cause cellulitis, impetigo, or abscesses.
Chronic or Recurrent Infection
Incomplete treatment, reinfection, or persistent risk factors (e.g., poor hygiene, immunosuppression) can lead to long-standing or frequently recurring infections.
Kerion Formation (in Tinea Capitis)
A severe inflammatory reaction resulting in a painful, boggy mass with pus and hair loss
May result in permanent scarring and irreversible alopecia (hair loss)
Nail Deformity (in Tinea Unguium)
Chronic infection of the nail can cause permanent changes in nail shape, thickness, or color
May affect function and appearance
Spread to Other Body Areas or Individuals
The infection may extend to adjacent skin or spread to other people through direct contact or shared items
Post-inflammatory Hyperpigmentation or Hypopigmentation
After healing, affected skin may remain discolored for a period, especially in individuals with darker skin tones
Psychosocial Impact
Visible lesions (especially on the face, scalp, or nails) may lead to embarrassment, social anxiety, or decreased self-esteem
Treatment
1. Topical Antifungal Therapy
Used for mild to moderate, localized infections (e.g., tinea corporis, cruris, pedis):
Azoles:
Clotrimazole
Miconazole
Ketoconazole
Econazole
Allylamines:
Terbinafine (more effective than azoles)
Naftifine
Butenafine
Others:
Ciclopirox
Tolnaftate
Duration: Usually 2–4 weeks (continue 1 week after symptom resolution)
2. Oral Antifungal Therapy
Used for extensive, chronic, or refractory infections, or when hair or nails are involved:
Terbinafine
First-line for tinea unguium and capitis
Duration:
Skin: ~2 weeks
Nails: 6 weeks (fingernails), 12 weeks (toenails)
Griseofulvin
Especially used in tinea capitis in children
Long duration: 6–8 weeks or more
Itraconazole
Alternative for nail and skin infections
Can be used as pulse therapy for onychomycosis
Fluconazole
Also used for tinea and candidiasis
Weekly dosing possible for nails
3. Adjunctive Measures
Keep affected area clean and dry
Avoid tight clothing and occlusive footwear
Do not share personal items (e.g., towels, combs, shoes)
Treat household contacts or pets if source of infection
Use antifungal powders or sprays in recurrent tinea pedis
4. Treatment of Inflammatory or Secondary Infections
Topical corticosteroids: Only in combined antifungal/steroid creams for short-term use in highly inflamed cases
Antibiotics: If there’s a secondary bacterial infection