Castleman Disease
Content of This Page
1- Introduction
2- Pathophysiology
3- Classification of Castleman Disease
4- Epidemiology and Risk Factors
5- Clinical Features
6- Investigations
7- Treatment
8- Prognosis & Follow-up
9- Castleman Disease in HIV and HHV-8 Infection
Introduction
Castleman Disease (CD) is a rare, non-clonal lymphoproliferative disorder characterized by abnormal growth of lymphoid tissue. First described by Dr. Benjamin Castleman in the 1950s, it represents a heterogeneous group of conditions that share similar histopathological features but differ widely in clinical presentation, pathogenesis, and prognosis. It is classified into:
Unicentric Castleman Disease (UCD): Affects a single lymph node region, often asymptomatic, and usually curable with surgery.
Multicentric Castleman Disease (MCD): Involves multiple lymph nodes with systemic symptoms; may be linked to HHV-8 or occur idiopathically.
Pathophysiology
1. Unicentric Castleman Disease (UCD):
The exact cause is unclear, but it is thought to result from a localized, reactive lymph node hyperplasia.
Abnormal follicular dendritic cell (FDC) proliferation and increased vascularity are common histologic findings.
Interleukin-6 (IL-6) may be locally elevated but is usually not systemically increased.
2. Multicentric Castleman Disease (MCD):
MCD is driven by chronic systemic inflammation, often mediated by elevated IL-6 levels, leading to widespread lymphoid hyperplasia and systemic symptoms.
a. HHV-8-associated MCD:
Common in HIV-positive individuals.
HHV-8 infects B cells and promotes excessive IL-6 and viral IL-6 (vIL-6) production.
This leads to systemic inflammation, angiogenesis, and immune dysregulation.
b. Idiopathic MCD (iMCD):
Occurs without HHV-8 or HIV infection.
Cause remains uncertain, but IL-6 is a key driver.
Likely involves autoimmune, autoinflammatory, or neoplastic mechanisms.
Some cases show involvement of plasmablasts or clonal expansions of immune cells.
Key Mediators:
Interleukin-6 (IL-6): Central to both MCD and, to a lesser extent, UCD.
Vascular Endothelial Growth Factor (VEGF): Contributes to angiogenesis and lymph node enlargement.
B-cell and plasma cell activation: Drives lymph node hyperplasia and systemic symptoms.

Classification of Castleman Disease
1. Clinical Classification:
A. Unicentric Castleman Disease (UCD):
Involves a single lymph node region.
Often asymptomatic or causes local symptoms due to mass effect.
Usually has a benign course and is curable with surgical excision.
B. Multicentric Castleman Disease (MCD):
Involves multiple lymph node regions.
Associated with systemic inflammatory symptoms such as fever, weight loss, and fatigue.
Further subdivided into:
HHV-8-associated MCD (typically in HIV-positive patients)
Idiopathic MCD (iMCD) (no evidence of HHV-8 or HIV)
POEMS-associated MCD (seen in patients with POEMS syndrome)
2. Histopathological Classification:
Regardless of clinical type, lymph node biopsy in CD may show one of the following patterns:
A. Hyaline Vascular Type:
Most common in UCD.
Characterized by small hyalinized follicles and prominent vascular proliferation.
B. Plasma Cell Type:
Common in MCD.
Shows hyperplastic germinal centers and sheets of plasma cells in interfollicular zones.
C. Mixed Type:
Features of both hyaline vascular and plasma cell types.
3. Etiologic Classification (Specific to MCD):
| Subtype | Association |
|---|---|
| HHV-8-associated MCD | HIV-positive or immunocompromised |
| Idiopathic MCD (iMCD) | Unknown cause, often autoimmune-like |
| POEMS-associated MCD | Linked to POEMS syndrome |
Epidemiology and Risk Factors
Epidemiology:
1. General Prevalence:
Castleman Disease (CD) is rare, with an estimated incidence of:
UCD: ~15–30 cases per million per year.
MCD: Less common but more severe; precise global incidence is unclear due to underdiagnosis.
2. Age and Gender:
Unicentric CD (UCD):
Can occur at any age.
Most commonly diagnosed in young adults (20–40 years).
Slight female predominance.
Multicentric CD (MCD):
Typically affects middle-aged to older adults.
HHV-8-associated MCD is more frequent in HIV-positive men, especially in their 30s–50s.
Idiopathic MCD (iMCD) affects both genders equally.
3. Geographical Distribution:
HHV-8-associated MCD is more common in areas with high HIV or HHV-8 prevalence, such as:
Sub-Saharan Africa
Parts of the Mediterranean
Some regions in Asia and Latin America
Risk Factors:
1. Viral Infections:
Human Herpesvirus 8 (HHV-8):
Strongly associated with HHV-8-associated MCD.
Viral IL-6 mimics human IL-6, driving disease pathogenesis.
HIV Infection:
Increases the risk of HHV-8 infection and MCD development.
2. Immunosuppression:
Immunocompromised individuals, especially those with HIV/AIDS or on immunosuppressive therapy, are at higher risk of MCD.
3. Autoimmune Conditions (iMCD):
Some idiopathic MCD cases may be associated with autoimmune or autoinflammatory processes.
Exact triggers are unclear but may involve dysregulated cytokine production, especially IL-6.
4. POEMS Syndrome:
A rare paraneoplastic disorder involving polyneuropathy, organomegaly, endocrinopathy, monoclonal plasma cell disorder, and skin changes.
Associated with a subset of MCD cases.
Clinical Features
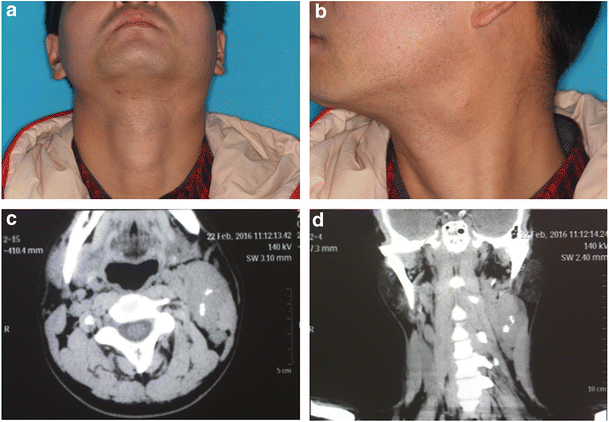
Unicentric Castleman Disease (UCD):
Usually asymptomatic or causes localized symptoms due to an enlarged lymph node (e.g., neck mass, cough, abdominal discomfort). Systemic symptoms are rare.Multicentric Castleman Disease (MCD):
Causes systemic symptoms such as fever, night sweats, fatigue, weight loss, and generalized lymphadenopathy. Patients may also have hepatosplenomegaly, anemia, elevated inflammatory markers, and polyclonal hypergammaglobulinemia.
POEMS-associated MCD includes additional features like polyneuropathy, endocrine disorders, and skin changes.
Investigations
Blood Tests:
Show anemia, elevated inflammatory markers (CRP, ESR), high IL-6, and polyclonal hypergammaglobulinemia—especially in Multicentric CD (MCD).Viral Testing:
Check for HIV and HHV-8 to assess risk for HHV-8–associated MCD.Imaging:
CT or PET-CT scans help identify lymphadenopathy, organ enlargement, and distinguish between Unicentric (UCD) and Multicentric (MCD) types.Lymph Node Biopsy (Excisional):
Essential for diagnosis; shows hyaline vascular, plasma cell, or mixed patterns.
Bone Marrow Biopsy:
Done in MCD to assess plasma cell involvement or POEMS syndrome features.
Treatment
Unicentric Castleman Disease (UCD):
Surgical excision is the treatment of choice and usually curative.
Radiotherapy is used if surgery isn’t possible.
Multicentric Castleman Disease (MCD):
HHV-8–associated MCD:
Rituximab (with or without chemotherapy)
Antiviral therapy and HIV treatment (cART) if HIV-positive
Idiopathic MCD (iMCD):
Anti–IL-6 therapy (Siltuximab or Tocilizumab)
Corticosteroids or immunosuppressants if needed
POEMS-associated MCD:
Treat underlying plasma cell disorder (e.g., chemotherapy or stem cell transplant)
Supportive care includes managing anemia, infections, and inflammation.
Treatment is tailored based on disease type and underlying causes.
Prognosis & Follow-up
Unicentric Castleman Disease (UCD):
Excellent prognosis with surgical removal (5-year survival >95%).
Rarely recurs.
Follow-up: Annual clinical checks; imaging only if needed.
Multicentric Castleman Disease (MCD):
Variable prognosis, depending on the subtype:
HHV-8–associated: Improved with rituximab and HIV therapy.
Idiopathic MCD: May relapse or progress; response to IL-6 therapy varies.
POEMS-associated: Outcome depends on treatment of plasma cell disorder.
Follow-up: Every 3–6 months with physical exams, labs (CBC, CRP, IL-6), and imaging.
Castleman Disease in HIV and HHV-8 Infection
HHV-8–associated Multicentric Castleman Disease (MCD) is common in HIV-positive individuals.
Caused by HHV-8 infection of B-cells, leading to overproduction of viral IL-6 and systemic inflammation.
Symptoms: Fever, night sweats, lymphadenopathy, hepatosplenomegaly, and cytopenias.
Diagnosis: Lymph node biopsy and detection of HHV-8 (via PCR or immunohistochemistry).
Treatment:
cART (HIV control)
Rituximab (first-line therapy)
Chemotherapy for severe or refractory cases
Prognosis: Good with proper treatment; poor if untreated or immunosuppressed.