Breast Cancer
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- Prevention and Early Detection
Introduction
Breast cancer is a type of cancer that originates in the cells of the breast, most commonly in the lining of the milk ducts or the lobules that supply the ducts with milk. It can affect both men and women, though it is far more common in women.

Causes
1. Genetic Factors:
- Inherited Gene Mutations: Mutations in certain genes, such as BRCA1 and BRCA2, can significantly increase the risk of developing breast cancer. These mutations can be inherited from either parent.
- Family History: Having close relatives (mother, sister, daughter) with breast cancer increases the likelihood of developing the disease. This is often related to inherited genetic mutations.
2. Hormonal Factors:
- Estrogen and Progesterone Exposure: Prolonged exposure to estrogen and progesterone hormones, due to early menstruation (before age 12), late menopause (after age 55), or hormone replacement therapy (HRT), can increase breast cancer risk.
- Reproductive History: Women who have never been pregnant, or who had their first pregnancy after the age of 30, may have a slightly higher risk of breast cancer due to longer exposure to hormones.
3. Environmental and Lifestyle Factors:
- Radiation Exposure: Previous exposure to radiation therapy, especially in the chest area during adolescence or young adulthood, increases breast cancer risk.
- Alcohol Consumption: Regular alcohol consumption is linked to an increased risk of breast cancer. The risk increases with the amount of alcohol consumed.
- Obesity: Being overweight, especially after menopause, can increase the risk of breast cancer. Fat tissue produces estrogen, which can contribute to the development of hormone-receptor-positive breast cancer.
- Physical Inactivity: Lack of regular physical activity is associated with an increased risk of breast cancer.
4. Age and Gender:
- Age: The risk of breast cancer increases as a woman gets older, particularly after age 50.
- Gender: Being female is the most significant risk factor, as breast cancer is much more common in women than in men.
5. Other Factors:
- Dense Breast Tissue: Women with dense breast tissue have a higher risk of breast cancer. Dense tissue can also make it harder to detect cancers on mammograms.
- Personal History of Breast Cancer: Women who have had breast cancer in one breast have an increased risk of developing cancer in the other breast or in another part of the same breast.
- Certain Benign Breast Conditions: Some non-cancerous breast conditions, like atypical hyperplasia, are associated with an increased risk of breast cancer.
6. Lifestyle Choices:
- Diet: Diets high in saturated fats and low in fruits and vegetables may increase the risk of breast cancer, though the exact relationship is still under investigation.
- Smoking: Some studies suggest a link between smoking and an increased risk of breast cancer, particularly in premenopausal women.
7. Ethnicity and Race:
- Ethnicity: Breast cancer is slightly more common in Caucasian women compared to African American, Hispanic, and Asian women. However, African American women are more likely to develop aggressive types of breast cancer at a younger age.
8. Breastfeeding and Childbearing:
- Breastfeeding: Women who breastfeed, especially for over a year, may have a slightly reduced risk of breast cancer. The protective effect is likely due to hormonal changes that occur during breastfeeding.
Symptoms
1. Lump or Mass in the Breast
- The most common symptom of breast cancer is a new lump or mass in the breast. These lumps are often hard, irregular in shape, and painless, though some may be tender or soft.
2. Changes in Breast Shape or Size
- Any unexplained change in the size, shape, or appearance of the breast, including swelling, may indicate breast cancer.
3. Nipple Changes
- Inversion (turning inward) of the nipple.
- Discharge from the nipple, which may be clear, bloody, or another color.
- Changes in the skin of the nipple, such as redness, scaliness, or thickening.
4. Skin Changes
- Dimpling or puckering of the skin, resembling the texture of an orange peel.
- Redness, scaling, or thickening of the skin on the breast or nipple.
5. Breast or Nipple Pain
- While breast pain is often associated with benign conditions, persistent pain or discomfort in one area of the breast should be evaluated by a healthcare provider.
6. Swelling or Lumps in the Armpit
- Swelling or lumps in the lymph nodes under the arm or around the collarbone may be a sign that breast cancer has spread.
7. Unexplained Weight Loss or Fatigue
- In more advanced stages, breast cancer can cause systemic symptoms like unexplained weight loss or persistent fatigue.
8. Visible Changes
- Veins becoming more prominent on the surface of the breast.
Stages of The Disease
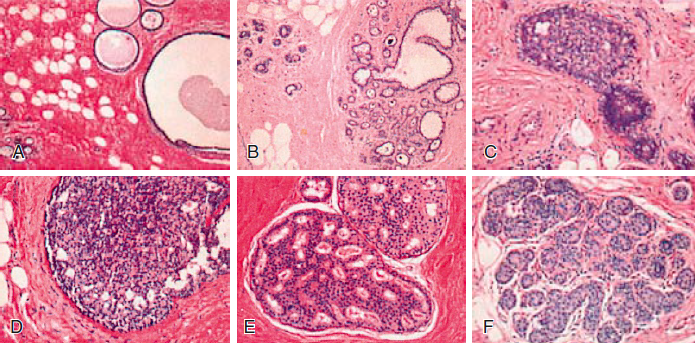
-Stage 0 (Carcinoma in Situ)
- Ductal Carcinoma in Situ (DCIS): In this stage, the cancer cells are confined within the ducts of the breast and have not invaded surrounding breast tissue. It is considered non-invasive but requires treatment to prevent progression.
-Stage I (Early Stage)
- Stage IA: The tumor is 2 cm or smaller and has not spread outside the breast. There is no involvement of lymph nodes.
- Stage IB: Small clusters of cancer cells are found in the lymph nodes, and either there is no primary tumor in the breast or the tumor is 2 cm or smaller.
-Stage II (Localized Advanced Stage)
- Stage IIA:
- No tumor is found in the breast, but cancer is found in 1 to 3 axillary lymph nodes (nodes under the arm).
- The tumor is 2 to 5 cm and may or may not have spread to the axillary lymph nodes.
- Stage IIB:
- The tumor is larger than 5 cm but has not spread to the axillary lymph nodes.
- The tumor is 2 to 5 cm and has spread to 1 to 3 axillary lymph nodes.
-Stage III (Locally Advanced Stage)
- Stage IIIA:
- The tumor is larger than 5 cm and has spread to 1 to 3 axillary lymph nodes or to internal mammary lymph nodes (near the breastbone).
- The tumor is any size with cancer spread to 4 to 9 axillary lymph nodes or internal mammary lymph nodes.
- Stage IIIB:
- The tumor has invaded the chest wall or skin of the breast, causing swelling or ulceration. It may or may not have spread to lymph nodes.
- Stage IIIC:
- The tumor can be of any size and has spread to 10 or more axillary lymph nodes, or to lymph nodes above or below the collarbone, or to internal mammary lymph nodes.
-Stage IV (Metastatic Breast Cancer)
- At this stage, the cancer has spread beyond the breast and nearby lymph nodes to other parts of the body, such as the bones, liver, lungs, or brain. This stage is also known as metastatic or advanced breast cancer.
-Recurrent Breast Cancer
- This is not a stage, but it refers to cancer that has returned after treatment. It can recur locally in the breast or chest wall, or distantly in other parts of the body.
Treatment
1. Surgery
- Lumpectomy (Breast-Conserving Surgery): Involves removing the tumor and a small margin of surrounding healthy tissue. It’s often followed by radiation therapy.
- Mastectomy: Removal of the entire breast. In some cases, a double mastectomy (removal of both breasts) may be recommended, especially if there’s a high genetic risk.
- Sentinel Lymph Node Biopsy: A surgical procedure to remove and examine the first few lymph nodes (sentinel nodes) where cancer might spread.
- Axillary Lymph Node Dissection: If cancer is found in the sentinel nodes, additional lymph nodes in the armpit may be removed.
2. Radiation Therapy
- External Beam Radiation: High-energy beams are directed at the breast or chest wall to kill cancer cells. It is commonly used after surgery to reduce the risk of recurrence.
- Brachytherapy (Internal Radiation): Radioactive seeds are placed inside or near the tumor site, offering a more targeted approach.
3. Chemotherapy
- Involves the use of drugs to destroy cancer cells or slow their growth. Chemotherapy can be administered before surgery (neoadjuvant therapy) to shrink tumors, or after surgery (adjuvant therapy) to kill any remaining cancer cells.
- It is also used in cases of advanced or metastatic breast cancer.
4. Hormone (Endocrine) Therapy
- Tamoxifen: A drug that blocks estrogen receptors on breast cancer cells, commonly used in premenopausal women.
- Aromatase Inhibitors: Drugs like anastrozole, letrozole, and exemestane, which lower estrogen levels by blocking the enzyme aromatase. These are typically used in postmenopausal women.
- Ovarian Suppression: In premenopausal women, treatments may include medications or surgery to suppress or remove the ovaries, reducing estrogen production.
5. Targeted Therapy
- HER2-Targeted Therapy: For cancers that overexpress the HER2 protein. Drugs like trastuzumab (Herceptin), pertuzumab, and ado-trastuzumab emtansine specifically target HER2-positive cancer cells.
- CDK4/6 Inhibitors: Drugs like palbociclib, ribociclib, and abemaciclib, often used in combination with hormone therapy to treat HR-positive, HER2-negative breast cancer.
6. Immunotherapy
- Checkpoint Inhibitors: Drugs like pembrolizumab (Keytruda) are used to enhance the immune system’s ability to recognize and attack cancer cells. Immunotherapy is primarily used for triple-negative breast cancer.
7. Bone-Directed Therapy
- In cases where breast cancer has spread to the bones, drugs like bisphosphonates (e.g., zoledronic acid) or denosumab are used to strengthen bones and reduce the risk of fractures.
8. Clinical Trials
- Patients may be eligible for clinical trials that offer access to new and experimental treatments.
Prevention And Early Detection
-Prevention :-
While not all breast cancer cases can be prevented, certain lifestyle changes and medical interventions can reduce the risk:
Lifestyle Changes
- Maintain a Healthy Weight: Being overweight or obese, especially after menopause, increases the risk of breast cancer.
- Exercise Regularly: Engaging in regular physical activity helps maintain a healthy weight and may lower the risk.
- Limit Alcohol Consumption: Alcohol intake is linked to an increased risk of breast cancer. Limiting alcohol to one drink per day or less is recommended.
- Healthy Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins, and low in processed foods and red meat, may reduce cancer risk.
- Avoid Smoking: Smoking is linked to many types of cancer, including breast cancer.
Hormonal Considerations
- Limit Postmenopausal Hormone Therapy: Combination hormone therapy (estrogen and progesterone) for more than three to five years increases breast cancer risk. If hormone therapy is necessary, it should be used at the lowest dose and for the shortest time possible.
- Breastfeed if Possible: Breastfeeding for several months may slightly reduce breast cancer risk, especially for women with a family history of the disease.
Medical Interventions
- Medications: In some high-risk women, doctors may recommend preventive medications such as selective estrogen receptor modulators (SERMs) like tamoxifen or raloxifene, or aromatase inhibitors.
- Prophylactic Surgery: For women with a very high risk of breast cancer (e.g., those with BRCA1 or BRCA2 gene mutations), prophylactic mastectomy (removal of the breasts) or oophorectomy (removal of the ovaries) may be considered to significantly reduce risk.
-Early Detection :-
Early detection of breast cancer increases the chances of successful treatment. The following methods are key to early detection:
Breast Self-Examination (BSE)
- Women should become familiar with the normal look and feel of their breasts to detect any changes. While BSEs are no longer universally recommended for all women, being aware of any changes in the breasts can be an important first step.
Clinical Breast Examination (CBE)
- A healthcare provider can perform a physical exam of the breasts to check for lumps or other changes. CBEs are often done as part of routine physical exams.
Mammography
- Screening Mammograms: These X-rays of the breast are the most effective tool for early detection of breast cancer. Regular mammograms can detect cancer before symptoms appear.
- Age 40-49: Women should discuss the risks and benefits of starting mammograms with their healthcare provider, as some organizations recommend starting at age 40.
- Age 50-74: Most organizations recommend that women have a mammogram every 1 to 2 years.
- Age 75 and Older: Screening should continue based on the individual’s health and personal preferences.
- Screening Mammograms: These X-rays of the breast are the most effective tool for early detection of breast cancer. Regular mammograms can detect cancer before symptoms appear.
Magnetic Resonance Imaging (MRI)
- For women at high risk of breast cancer (e.g., those with BRCA mutations or a strong family history), MRI in addition to mammography is recommended for early detection.
Genetic Testing and Counseling
- Women with a family history of breast or ovarian cancer should consider genetic testing for mutations in the BRCA1 and BRCA2 genes. If a mutation is found, they can work with their healthcare team to create a personalized risk-reduction plan.
Regular Medical Checkups
- Regular checkups with a healthcare provider can help with the early detection of breast cancer, especially for women who are at increased risk.