Prostatitis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of Prostatitis
5- Treatment
6- What Should You Avoid
Introduction
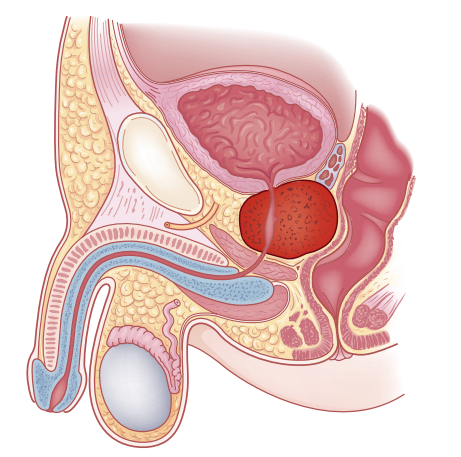
Prostatitis is an inflammation of the prostate gland, which is located just below the bladder and surrounds the urethra in men. This condition can affect men of all ages and can lead to a variety of symptoms, including pelvic pain, discomfort during urination, and sexual dysfunction.
Causes
1. Acute Bacterial Prostatitis
- Bacterial Infection: Caused by bacteria, commonly Escherichia coli (E. coli), that enter the prostate gland. These bacteria usually originate from the urinary tract or other parts of the body.
2. Chronic Bacterial Prostatitis
- Persistent Bacterial Infection: A prolonged bacterial infection that is often harder to detect and treat. It may occur if an initial infection is not fully eradicated or if there is an ongoing source of bacteria.
3. Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
- Non-Bacterial Causes: The exact cause is often unknown, but possible factors include:
- Autoimmune Reactions: The immune system may mistakenly attack the prostate tissue.
- Nerve Damage: Injury or irritation of the nerves around the prostate may contribute to pain.
- Pelvic Floor Dysfunction: Muscle tension or dysfunction in the pelvic floor can cause chronic pain.
- Inflammatory Response: Chronic inflammation without a clear bacterial cause.
4. Asymptomatic Inflammatory Prostatitis
- Unknown Causes: Inflammation occurs without any noticeable symptoms. It is often discovered incidentally during tests for other conditions.
Symptoms
1. Acute Bacterial Prostatitis
- High Fever and Chills: Sudden onset of fever and chills.
- Severe Pelvic Pain: Intense pain in the lower abdomen, pelvis, or perineum (area between the scrotum and rectum).
- Painful Urination: Pain or burning sensation during urination.
- Frequent Urination: Urgent need to urinate frequently.
- Difficulty Urinating: Pain or difficulty starting or maintaining urine flow.
- Nausea and Vomiting: Possible gastrointestinal symptoms.
2. Chronic Bacterial Prostatitis
- Persistent Pelvic Pain: Ongoing pain in the pelvic area.
- Discomfort During Urination: Pain or discomfort while urinating.
- Frequent Urination: Increased need to urinate, especially at night.
- Pain During Ejaculation: Pain or discomfort during or after ejaculation.
3. Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
- Chronic Pelvic Pain: Long-term pain in the pelvic region that is not related to a bacterial infection.
- Discomfort During Urination: Pain or discomfort while urinating.
- Frequent Urination: Urgent need to urinate, which can be frequent.
- Pain During Ejaculation: Discomfort or pain during or after ejaculation.
- Lower Back Pain: Some individuals may experience pain in the lower back or hips.
4. Asymptomatic Inflammatory Prostatitis
- No Noticeable Symptoms: Often discovered incidentally during medical exams for other conditions.
- No Pain or Discomfort: Typically does not present with any symptoms.
Stages of Prostatitis
1. Acute Bacterial Prostatitis
- Description: This is the initial and most severe stage of prostatitis. It involves a sudden bacterial infection of the prostate.
- Symptoms: Severe pelvic pain, high fever, chills, painful urination, frequent urination, and nausea.
- Treatment: Requires immediate antibiotic therapy, often administered intravenously in a hospital setting, along with pain management.
2. Chronic Bacterial Prostatitis
- Description: This stage is characterized by a long-term bacterial infection that persists despite treatment. It can be difficult to diagnose and manage.
- Symptoms: Chronic pelvic pain, discomfort during urination, frequent urination, and pain during ejaculation.
- Treatment: Long-term antibiotics are usually needed, along with regular monitoring to manage symptoms and prevent recurrence.
3. Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
- Description: This is the most common form of prostatitis and is not caused by a bacterial infection. It is classified into subtypes based on symptoms and inflammation:
- Type I: Inflammatory, with evidence of bacteria present.
- Type II: Inflammatory, without evidence of bacteria.
- Type III: Non-inflammatory, with chronic pelvic pain but no infection.
- Type IV: Asymptomatic inflammatory prostatitis, discovered incidentally.
- Symptoms: Chronic pelvic pain, frequent urination, discomfort during urination and ejaculation.
- Treatment: Aims to relieve symptoms and may include pain management, physical therapy, and lifestyle changes.
4. Asymptomatic Inflammatory Prostatitis
- Description: Inflammation of the prostate without noticeable symptoms. It is often detected incidentally during tests for other conditions.
- Symptoms: None, as it does not present with symptoms.
- Treatment: Typically requires no treatment unless associated with other conditions.
5. Chronic Interstitial Prostatitis
- Description: A severe and prolonged form of prostatitis where inflammation leads to chronic pain and potential long-term damage to the prostate tissue.
- Symptoms: Persistent pelvic pain, urinary discomfort, and sexual dysfunction.
- Treatment: Focuses on managing symptoms and may include medications, physical therapy, and, in severe cases, surgical interventions.
Treatment
1. Acute Bacterial Prostatitis
- Antibiotics: Immediate treatment with intravenous antibiotics to target the bacterial infection. Oral antibiotics may follow.
- Pain Relievers: Medications like nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation.
- Hydration: Increased fluid intake to help flush out bacteria.
- Hospitalization: Often required for severe cases to manage symptoms and administer treatment.
2. Chronic Bacterial Prostatitis
- Long-Term Antibiotics: Extended courses of oral antibiotics to fully eradicate the infection. The choice of antibiotic may be adjusted based on urine culture results.
- Pain Management: NSAIDs or other pain relievers to manage chronic pain.
- Follow-Up Care: Regular monitoring to ensure the infection is fully resolved and to manage any ongoing symptoms.
3. Chronic Prostatitis/Chronic Pelvic Pain Syndrome (CP/CPPS)
- Pain Relief: NSAIDs or other pain medications to alleviate discomfort.
- Alpha-Blockers: Medications like tamsulosin to relax the muscles around the prostate and bladder neck, improving urine flow.
- Physical Therapy: Pelvic floor physical therapy to address muscle tension and improve pelvic health.
- Lifestyle Modifications: Dietary changes, stress management, and avoiding irritants like caffeine and alcohol.
- Medications: Other medications, such as muscle relaxants or antidepressants, may be used based on symptoms.
4. Asymptomatic Inflammatory Prostatitis
- Observation: Typically no treatment is required unless the inflammation is associated with other health issues.
- Monitoring: Regular check-ups to ensure no complications arise or to manage any incidental findings.
5. Chronic Interstitial Prostatitis
- Symptom Management: Pain management strategies, including NSAIDs, muscle relaxants, and physical therapy.
- Bladder Instillations: Treatments where medication is directly placed into the bladder to relieve symptoms.
- Lifestyle Adjustments: Changes in diet and daily habits to manage symptoms.
- Surgical Options: In severe cases, procedures or surgeries may be considered to address underlying issues or manage symptoms.
General Tips for Managing Prostatitis:
- Stay Hydrated: Drink plenty of fluids to support urinary health.
- Avoid Irritants: Limit intake of caffeine, alcohol, and spicy foods.
- Regular Follow-Up: Keep up with medical appointments to monitor progress and adjust treatment as needed.
What Should You Avoid
To manage prostatitis effectively and alleviate symptoms, consider avoiding the following:
1. Caffeine
- Why Avoid: Can irritate the bladder and exacerbate urinary symptoms.
- Alternatives: Opt for non-caffeinated beverages like herbal teas or water.
2. Alcohol
- Why Avoid: Can increase inflammation and worsen symptoms.
- Alternatives: Stick to non-alcoholic drinks and stay hydrated with water.
3. Spicy Foods
- Why Avoid: Can irritate the urinary tract and prostate.
- Alternatives: Choose mild, non-spicy foods to avoid aggravating symptoms.
4. Acidic Foods and Drinks
- Why Avoid: Foods like citrus fruits and tomato-based products can irritate the bladder.
- Alternatives: Opt for non-acidic fruits and vegetables to avoid irritation.
5. Tight Clothing
- Why Avoid: Can trap moisture and increase discomfort.
- Alternatives: Wear loose-fitting, breathable clothing to maintain comfort.
6. Excessive Sitting
- Why Avoid: Prolonged sitting can increase pelvic pressure and discomfort.
- Alternatives: Take regular breaks to stand up and stretch, especially if sitting for long periods.
7. Straining During Bowel Movements
- Why Avoid: Can increase pressure on the prostate and exacerbate symptoms.
- Alternatives: Ensure a high-fiber diet to prevent constipation and avoid straining.
8. Sexual Activity
- Why Avoid: May exacerbate symptoms or discomfort in some cases.
- Alternatives: Consult with a healthcare provider for personalized advice on managing symptoms related to sexual activity.
9. Irritating Personal Care Products
- Why Avoid: Scented soaps, bubble baths, and other products can irritate the genital area.
- Alternatives: Use mild, unscented personal care products.