Polycythemia Vera (PV)
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
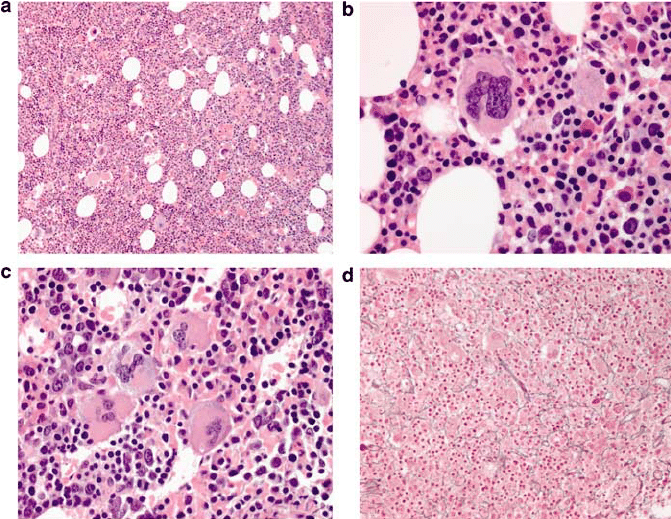
Polycythemia Vera (PV) is a rare blood disorder characterized by the overproduction of red blood cells in the bone marrow. This excess of red blood cells thickens the blood, leading to slower blood flow and an increased risk of clots. PV is classified as a type of myeloproliferative neoplasm (MPN), which means it’s a disorder where the bone marrow produces too many cells.
Causes
JAK2 Gene Mutation: The primary cause of PV is a mutation in the JAK2 gene, specifically the JAK2 V617F mutation.
Overproduction of Blood Cells: The JAK2 mutation leads to uncontrolled production of red blood cells, and sometimes white blood cells and platelets, in the bone marrow.
Acquired Mutation: The JAK2 mutation is acquired during a person’s lifetime and is not inherited from parents.
Overactive Signaling Pathways: The mutation causes the signaling pathways that regulate blood cell growth to become overactive, leading to the excess production of cells.
Other Contributing Factors: Age and possibly environmental factors may contribute to the development of PV, although the JAK2 mutation is the main cause.
Symptoms
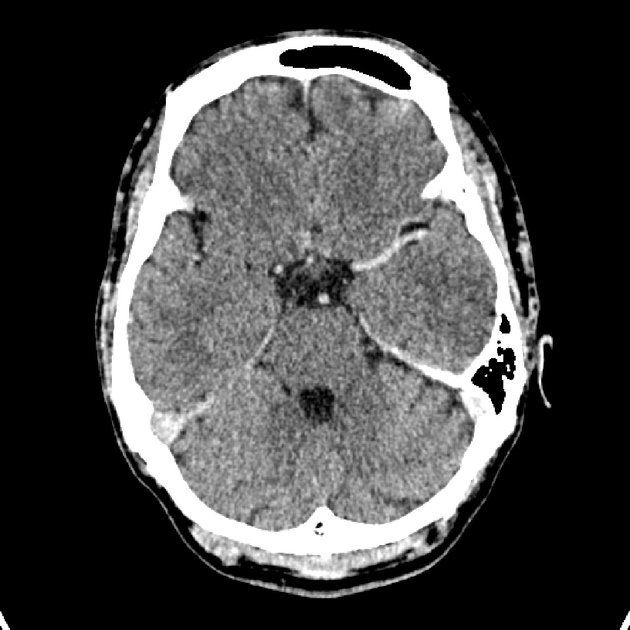
Headaches: Frequent or severe headaches are common due to increased blood thickness.
Dizziness or Lightheadedness: Caused by reduced blood flow due to the thicker blood.
Fatigue: Persistent tiredness and low energy levels are typical.
Itching (Pruritus): Intense itching, especially after a hot shower or bath.
Ruddy Complexion: A reddish or flushed appearance, particularly on the face, due to increased red blood cells.
Shortness of Breath: Difficulty breathing, especially during exertion.
Blurred Vision or Vision Problems: Due to reduced blood flow to the eyes.
Night Sweats: Excessive sweating during sleep.
Numbness or Tingling: Often in the hands and feet, due to poor circulation.
Unexplained Weight Loss: Some people may experience weight loss without trying.
Swelling or Pain in the Left Side of the Abdomen: Often due to an enlarged spleen (splenomegaly).
Blood Clots: Increased risk of clots, which can lead to complications like strokes, heart attacks, or deep vein thrombosis (DVT).
Stages of The Disease
1. Early Stage (Asymptomatic or Latent Phase)
- Characteristics: In this initial phase, many patients may not exhibit noticeable symptoms. PV might be discovered incidentally during routine blood tests showing elevated red blood cell counts.
- Symptoms: If present, symptoms are mild and might include fatigue or mild headaches.
- Blood Counts: There is a gradual increase in red blood cells, hemoglobin, and hematocrit levels.
2. Proliferative Stage (Symptomatic Phase)
- Characteristics: As the disease progresses, symptoms become more pronounced due to increased red blood cell production and blood viscosity.
- Symptoms: Common symptoms include headaches, dizziness, itching, and a ruddy complexion. There is a higher risk of developing blood clots.
- Blood Counts: Marked elevation in red blood cells, and possibly elevated white blood cells and platelets. Spleen enlargement (splenomegaly) may occur.
3. Spent Phase (Post-Polycythemic Myelofibrosis)
- Characteristics: In this advanced stage, the bone marrow becomes fibrotic (scarred), leading to a decrease in blood cell production.
- Symptoms: Anemia, fatigue, weight loss, and increased spleen size. Symptoms of myelofibrosis, such as bone pain and night sweats, may develop.
- Blood Counts: Blood counts may decrease due to marrow failure. The risk of progressing to acute myeloid leukemia (AML) increases, although this occurs in a minority of patients.
Treatment
1. Phlebotomy
- Description: Regular removal of blood from the body, similar to donating blood.
- Purpose: Reduces the number of red blood cells, decreasing blood thickness and the risk of clotting.
- Frequency: The frequency depends on individual needs, but it could range from once every few weeks to less often.
2. Medications
- Hydroxyurea: A chemotherapy drug used to suppress the bone marrow’s ability to produce blood cells, reducing red blood cell counts.
- Interferon-alpha: An immune-modulating drug that can reduce blood cell production and is often used in younger patients or during pregnancy.
- Ruxolitinib: A JAK2 inhibitor that specifically targets the JAK2 mutation, helping to reduce symptoms and control blood counts in patients who are resistant or intolerant to hydroxyurea.
- Aspirin: Low-dose aspirin is often prescribed to reduce the risk of blood clots by thinning the blood.
3. Managing Symptoms
- Itching: Antihistamines or ultraviolet light therapy may be used to relieve itching.
- Other Symptoms: Medications to address specific symptoms, like pain management for bone pain or fatigue.
4. Lifestyle Adjustments
- Avoiding Smoking: Smoking increases the risk of blood clots and should be avoided.
- Staying Active: Regular exercise can help improve circulation and reduce clot risk.
- Managing Cardiovascular Risk Factors: Controlling blood pressure, cholesterol, and diabetes is crucial.
5. Monitoring and Regular Checkups
- Regular blood tests to monitor red blood cell counts and adjust treatments as necessary.
- Ongoing evaluation for complications, such as blood clots, spleen enlargement, or progression to myelofibrosis or acute leukemia.
6. Bone Marrow Transplantation (Stem Cell Transplant)
- Consideration: This is a potential treatment for younger patients or those with advanced disease, though it carries significant risks and is not commonly used as a first-line treatment.
What Should You Avoid
Smoking: Increases the risk of blood clots and further thickens the blood.
Dehydration: Can thicken the blood even more; it’s important to stay well-hydrated.
Iron Supplements: Unless specifically recommended by a doctor, as they can stimulate red blood cell production, worsening PV.
Sedentary Lifestyle: Lack of movement can increase the risk of blood clots. Regular, moderate exercise is recommended.
Overheating: Hot showers, baths, and hot environments can worsen itching (pruritus).
High-Altitude Locations: May exacerbate symptoms due to lower oxygen levels, leading to increased red blood cell production.
Excessive Alcohol: Can affect blood clotting and exacerbate liver function, which may already be compromised in some PV patients.
Certain Medications: Avoid medications that increase clotting risk, like hormone replacement therapy (HRT) or some birth control pills, unless advised otherwise by a doctor.
Unmanaged Stress: Chronic stress can negatively impact overall health and potentially exacerbate symptoms.
Injury or Surgery Without Precaution: Increased risk of bleeding or clotting during surgeries; always inform healthcare providers of PV before any procedure.