Polymyositis
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Types of Disease
5- Treatment
6- What Should You Avoid
Introduction
Polymyositis is a rare inflammatory muscle disease that causes muscle weakness and inflammation. It primarily affects the muscles closest to the trunk, such as those in the shoulders, hips, and thighs. The condition can lead to progressive muscle weakness and discomfort. It is classified as an idiopathic inflammatory myopathy, meaning its exact cause is unknown.
Causes
- Autoimmune Reaction: Believed to be an autoimmune disorder where the immune system mistakenly attacks muscle tissues.
- Genetic Factors: Possible genetic predisposition, although no specific gene has been definitively linked.
- Environmental Triggers: Infections, certain medications, or other environmental factors might trigger or exacerbate the condition.
Symptoms
- Muscle Weakness: Gradual onset of weakness in the muscles closest to the trunk.
- Muscle Pain and Discomfort: Aching or soreness in affected muscles.
- Fatigue: General feeling of tiredness or lack of energy.
- Difficulty Swallowing: In some cases, weakness may extend to the muscles involved in swallowing (dysphagia).
- Respiratory Issues: Severe cases may affect respiratory muscles, leading to difficulty breathing.
Types of Disease
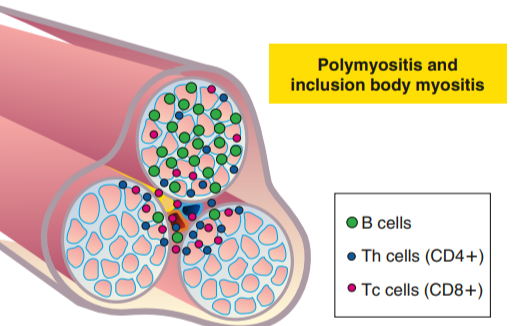
1. Polymyositis
- Description: A specific form of idiopathic inflammatory myopathy characterized by symmetric muscle weakness, typically affecting the proximal muscles (shoulders, hips, thighs).
- Characteristics: Progressive muscle weakness and inflammation without skin involvement.
2. Dermatomyositis
- Description: An inflammatory muscle disease that presents with both muscle weakness and characteristic skin rashes.
- Characteristics: Includes heliotrope rash (purple rash on the eyelids) and Gottron’s papules (red or violet papules over joints).
- Differences from Polymyositis: Dermatomyositis has prominent skin manifestations, whereas polymyositis typically does not.
3. Inclusion Body Myositis (IBM)
- Description: A progressive inflammatory muscle disease that often affects older adults. It is considered an idiopathic inflammatory myopathy with distinctive clinical and histological features.
- Characteristics: Muscle weakness and atrophy, particularly affecting the quadriceps and finger flexors. It is less responsive to conventional treatment compared to polymyositis.
- Differences from Polymyositis: IBM often presents with asymmetric muscle weakness and has a distinct histological pattern on muscle biopsy.
4. Juvenile Dermatomyositis
- Description: Dermatomyositis that occurs in children, typically under 18 years of age.
- Characteristics: Similar to adult dermatomyositis but with some variations in clinical presentation and potential for different complications.
5. Overlap Syndromes
- Description: Conditions that have features of polymyositis or dermatomyositis but also overlap with other autoimmune diseases.
- Examples:
- Scleromyositis: Features of both scleroderma and myositis.
- Mixed Connective Tissue Disease (MCTD): Includes features of systemic lupus erythematosus, scleroderma, and polymyositis.
6. Autoimmune Myositis Associated with Systemic Diseases
- Description: Inflammatory muscle disease that occurs in conjunction with other autoimmune conditions.
- Examples:
- Systemic Lupus Erythematosus (SLE): Can include myositis as a feature.
- Rheumatoid Arthritis: Myositis can be a complication of rheumatoid arthritis.
7. Necrotizing Autoimmune Myopathy
- Description: A rare form of autoimmune myopathy characterized by severe muscle damage and necrosis.
- Characteristics: Significant muscle weakness and damage, with elevated levels of muscle enzymes. It may be associated with autoantibodies such as anti-SRP or anti-HMGCR.

Treatment
Medications:
- Corticosteroids: Such as prednisone, to reduce inflammation and muscle weakness.
- Immunosuppressants: Medications like methotrexate or azathioprine may be used if corticosteroids are not effective or cause significant side effects.
- Biologics: Newer treatments such as rituximab or intravenous immunoglobulin (IVIG) may be considered in resistant cases.
Physical Therapy:
- Approach: To improve muscle strength, flexibility, and overall function.
- Focus: Customized exercise programs to maintain mobility and manage weakness.
Lifestyle Adjustments:
- Exercise: Low-impact exercises to maintain muscle strength and prevent atrophy.
- Diet: A balanced diet to support overall health and muscle function.
Management of Complications:
- Swallowing Difficulties: Dietary adjustments or feeding strategies if muscle weakness affects swallowing.
- Respiratory Support: In severe cases, respiratory therapy or support may be needed.
What Should You Avoid
1. Overexertion
- Avoid: Excessive physical activity or overexertion of muscles.
- Reason: Can worsen muscle weakness and lead to further damage. It’s important to balance exercise with rest.
2. Infections
- Avoid: Exposure to infectious agents, including viruses and bacteria.
- Reason: Infections can exacerbate symptoms and complicate treatment. Maintain good hygiene and seek medical care for any infections promptly.
3. Certain Medications
- Avoid: Medications that may trigger or worsen muscle symptoms.
- Examples: Statins (used to lower cholesterol) can sometimes contribute to muscle problems.
- Reason: Consult with a healthcare provider before starting any new medication, including over-the-counter drugs and supplements.
4. Excessive Sun Exposure
- Avoid: Prolonged or excessive sun exposure.
- Reason: Individuals with polymyositis, especially those with dermatomyositis, may have skin sensitivity that can be aggravated by sun exposure. Use sunscreen and protective clothing if you need to be outdoors.
5. Smoking and Alcohol
- Avoid: Smoking and excessive alcohol consumption.
- Reason: Smoking can impair circulation and overall health, while excessive alcohol can interfere with medication effectiveness and contribute to muscle weakness.
6. Uncontrolled Stress
- Avoid: High levels of stress and anxiety.
- Reason: Stress can negatively impact overall health and exacerbate symptoms. Practice stress-reduction techniques such as mindfulness, relaxation exercises, and counseling.
7. Unbalanced Diet
- Avoid: Diets high in processed foods, excessive sugar, or low in essential nutrients.
- Reason: A well-balanced diet supports overall health and can help manage symptoms. Ensure adequate intake of proteins, vitamins, and minerals, particularly those beneficial for muscle health.
8. Skipping Medications or Treatments
- Avoid: Missing doses of prescribed medications or skipping physical therapy sessions.
- Reason: Adherence to treatment plans is crucial for managing polymyositis and preventing symptom flare-ups.
9. Ignoring Symptoms
- Avoid: Neglecting new or worsening symptoms.
- Reason: Prompt reporting of changes in symptoms to a healthcare provider is essential for adjusting treatment and preventing complications.
10. Inappropriate Exercises
- Avoid: High-impact or strenuous exercises without guidance from a healthcare provider.
- Reason: Engage in a structured and supervised exercise program designed to maintain muscle function without causing further damage.
11. Autoimmune Triggers
- Avoid: Factors that may trigger or worsen autoimmune responses.
- Examples: Environmental toxins or other allergens that could potentially exacerbate the condition.