Thromboangiitis obliterans (TAO)
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Stages of The Disease
5- Treatment
6- What Should You Avoid
Introduction
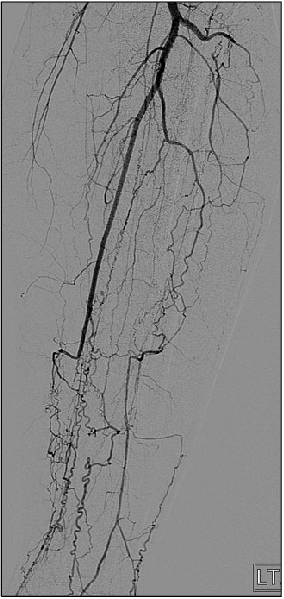
Thromboangiitis obliterans, also known as Buerger’s disease, is a rare, non-atherosclerotic inflammatory condition that affects small- and medium-sized arteries and veins, primarily in the extremities. It typically presents in young male smokers under the age of 45 and is strongly associated with tobacco use. The disease is characterised by a segmental pattern of inflammation and thrombosis (clot formation) within the vessels, leading to vascular occlusion and tissue ischaemia. Unlike atherosclerosis, which involves lipid deposition and plaque formation, thromboangiitis obliterans is driven by a cellular inflammatory process that results in thrombus formation and eventual obliteration of the vessel lumen. The condition most commonly affects the distal arteries of the hands and feet and may lead to symptoms such as claudication, rest pain, ulceration, and in advanced cases, gangrene. Early recognition and complete cessation of tobacco exposure are essential to prevent progression and limb loss.

Causes
-Primary Cause:
Tobacco use (most critical and consistent factor)
Cigarette smoking is strongly associated with the onset and progression of TAO.
It is also seen in users of chewing tobacco, bidi, and other forms of smokeless tobacco.
Cessation of tobacco use is essential to halt disease progression.
-Other Contributing Factors (less clearly defined):
Genetic predisposition:
More common in individuals from certain regions (e.g., South and Southeast Asia, Middle East).
HLA gene associations have been observed (e.g., HLA-B5, HLA-A9).
Immune mechanisms:
Evidence suggests an autoimmune component triggered by tobacco or endothelial injury.
Hypersensitivity to tobacco extracts and anti-endothelial cell antibodies have been found in some patients.
Infections:
Some theories propose a role for chronic infections, but this remains unproven.
Hypercoagulable states (rarely considered):
Though not a direct cause, may exacerbate vascular occlusion in susceptible individuals.
Symptoms
Claudication:
Pain in the feet, hands, or calves during exercise or walking.
Most commonly affects distal extremities (toes and fingers).
Rest Pain:
Pain in the affected limb even at rest, especially at night.
Indicative of critical limb ischemia.
Ulcers or Gangrene:
Non-healing ulcers on fingers or toes.
Can progress to dry or wet gangrene, often requiring amputation if untreated.
Superficial Thrombophlebitis:
Tender, inflamed superficial veins that may occur episodically.
Migratory and segmental in nature.
Cold Sensitivity and Numbness:
Affected limbs may feel cold, pale, and numb due to poor blood flow.
Color Changes and Skin Trophic Changes:
Skin may appear shiny, thin, or atrophic.
Loss of hair, brittle nails, and delayed capillary refill may be observed
Stages of The Disease
1. Preclinical / Subclinical Stage
Mild, nonspecific symptoms or asymptomatic.
Patients may have superficial thrombophlebitis or Raynaud’s phenomenon.
No overt signs of arterial occlusion.
Early vascular inflammation may be present.
2. Ischemic Stage (Early Clinical Stage)
Onset of intermittent claudication:
Pain in feet, legs, hands, or arms during exertion.
Most commonly in the plantar arch, calves, or forearms.
Cold sensitivity, numbness, and tingling.
Pulses may still be palpable in proximal arteries.
3. Critical Ischemia Stage
Rest pain (especially at night) due to severe ischemia.
Ulceration of fingers or toes begins.
Skin becomes pale, cold, shiny, and hairless.
Reduced or absent distal pulses.
4. Ulceration and Gangrene Stage (Advanced Disease)
Development of non-healing ischemic ulcers.
Progresses to dry or wet gangrene of fingers or toes.
High risk of superimposed infection.
May require amputation if revascularization is not possible and tobacco use continues.
Treatment
Absolute Smoking and Tobacco Cessation
This is the most critical and effective intervention.
Must include cessation of all forms of tobacco: cigarettes, bidis, chewing tobacco, and even passive smoke exposure.
Nicotine replacement therapy is generally avoided, as nicotine itself can aggravate the disease.
Referral to smoking cessation programs, behavioral therapy, and supportive counseling is strongly advised.
2. Medications (Supportive Role)
Vasodilators:
Examples: Nifedipine, Iloprost (a prostaglandin analog).
These help improve blood flow, reduce vasospasm, and alleviate rest pain.
Antiplatelet agents:
Such as aspirin or clopidogrel, to reduce the risk of thrombosis.
Analgesics:
Used for pain relief, especially in the rest pain or ulceration stage.
Pentoxifylline (optional use):
Improves red blood cell flexibility and microcirculatory flow.
3. Local Wound and Ulcer Care
Proper cleaning and dressing of ischemic ulcers.
Infection control with antibiotics if secondary infection is present.
Avoid trauma or pressure on affected areas.
4. Surgical and Interventional Options
Sympathectomy:
Can help in reducing rest pain and promoting ulcer healing in some cases.
Amputation:
Required in cases of irreversible gangrene or severe infection.
Aim for minimal and functional loss, preserving as much limb as possible.
Revascularization procedures:
Rarely effective, as the disease affects distal and segmental arteries, which are not suitable for bypass.
5. Patient Education and Support
Importance of permanent smoking cessation must be emphasized repeatedly.
Education on foot care, avoiding cold exposure, and early reporting of new symptoms is essential
What Should You Avoid
- Tobacco in any form (smoking, chewing, vaping, passive exposure)
- Nicotine-containing products (including nicotine patches or gum)
- Cold exposure (to prevent vasospasm)
- Tight or restrictive footwear
- Minor trauma to hands or feet
- Walking barefoot
- Infections (especially in ulcers or wounds)
- Sitting or standing for prolonged periods without movement
- Stress (which can worsen vasospasm)
- Alcohol (in excess, as it may worsen peripheral vasodilation and ulcers)
- Poor foot hygiene or neglect of wound care
- Self-medication or delay in seeking treatment for ulcers/gangrene