Non-Alcoholic Fatty Liver Disease (NAFLD)
content of this page
1- Introduction, Definition & Overview
2- Pathophysiology
3- Risk Factors
4-Epidemiology
5- Clinical Features
6- Investigations
7- Management
8- Prognosis
Introduction, Definition & Overview
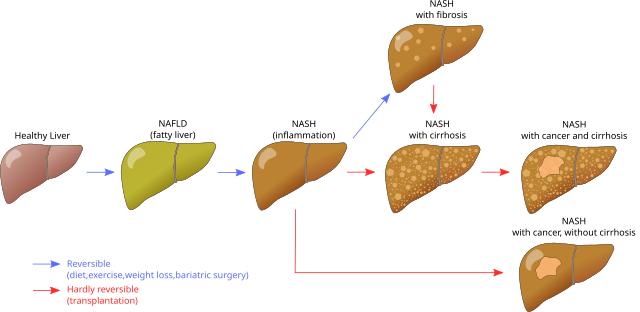
NAFLD is a spectrum of liver diseases characterized by hepatic fat accumulation (>5%) in individuals without significant alcohol consumption.
It ranges from:
Simple steatosis (fat only)
To non-alcoholic steatohepatitis (NASH) → inflammation ± ballooning ± fibrosis
Eventually leading to cirrhosis and hepatocellular carcinoma (HCC)
It’s considered the hepatic manifestation of metabolic syndrome.
Pathophysiology
NAFLD pathogenesis involves:
First hit: Insulin resistance → ↑ hepatic free fatty acids → steatosis
Second hits (progression to NASH/fibrosis):
Oxidative stress (free radicals)
Lipotoxicity
Cytokine release (e.g. TNF-α)
Gut-derived endotoxins
Endoplasmic reticulum stress
Genetic predisposition (e.g. PNPLA3)
Risk Factors
Obesity (especially central)
Type 2 diabetes
Dyslipidaemia
Hypertension
Polycystic ovary syndrome
Obstructive sleep apnoea
Sedentary lifestyle

Epidemiology
Affects ~24% globally
Present in:
94% of obese (BMI >30)
67% of overweight (BMI >25)
25% of normal BMI
Strong ethnic & gender variations
Clinical Features
Often asymptomatic
May cause fatigue, mild RUQ discomfort
Detected incidentally via:
Elevated liver enzymes (ALT > AST early on)
‘Bright liver’ on ultrasound
May present late with:
Cirrhosis (ascites, varices, encephalopathy)
Hepatocellular carcinoma
Investigations
Aim: Confirm steatosis, assess fibrosis, exclude other liver diseases
-Biochemistry
↑ GGT common
ALT/AST mildly raised
AST:ALT ratio inverts with advanced fibrosis
Ferritin may be elevated
ANA may be low-titre positive
-Fibrosis scores
NAFLD Fibrosis Score, FIB-4 → rule out advanced fibrosis
Enhanced Liver Fibrosis (ELF) panel (specialist use)
-Imaging
Ultrasound (low sensitivity <33% steatosis)
Transient Elastography (for fibrosis)
CAP (for fat content)
–Liver biopsy
Not routinely required
“Gold standard” for diagnosing NASH and assessing fibrosis
Management
Lifestyle is the cornerstone:
Weight loss (≥7–10%) improves steatosis and inflammation
Control of diabetes, dyslipidaemia, and hypertension
Avoid hepatotoxic drugs & alcohol
-Surveillance
HCC screening in cirrhotic patients
Cardiovascular risk assessment (leading cause of death)
-Referral
Patients with advanced fibrosis (FIB-4 >2.67 or TE >8kPa) should be referred to hepatology
Prognosis
Fibrosis stage is the key determinant of prognosis
Simple steatosis → benign
NASH with fibrosis → progressive disease
High risk of:
Liver-related events (cirrhosis, HCC)
Extrahepatic events (CV disease, cancer)
NAFLD is projected to become the leading indication for liver transplantation globally