Absence Seizures
Content of This Page
1- Introduction
2- Causes
3- Symptoms
4- Tyoes of Absence Seizures
5- Investigations & Lab Results
6- Complications
7- Treatment
8- Prognosis
Introduction
Absence seizures are a type of generalized non-motor seizure characterized by brief, sudden lapses in consciousness. Most commonly seen in children aged 4 to 10 years, these seizures often appear as sudden episodes where the child “blanks out” or “stares into space” for a few seconds, typically without any warning and without post-ictal confusion.
They are associated with generalized epilepsy syndromes, most notably Childhood Absence Epilepsy (CAE). Unlike convulsive seizures, absence seizures are non-convulsive and can go unnoticed for long periods, often being mistaken for inattentiveness or daydreaming in school settings.
These seizures are often triggered by hyperventilation, and the hallmark diagnostic feature on EEG is a 3 Hz spike-and-wave discharge. Though typically benign and self-limiting in childhood, timely diagnosis and treatment are crucial to prevent cognitive and behavioral impairments.

Causes
1. Idiopathic (Primary) Causes
These are the most common, especially in children:
Genetic predisposition
(Often a family history of epilepsy or seizures)Childhood Absence Epilepsy (CAE) – typically between ages 4–10
Juvenile Absence Epilepsy (JAE) – later onset in adolescence
Channelopathies – mutations in ion channels (e.g., T-type calcium channels) involved in neuronal excitability
2. Secondary (Symptomatic) Causes
Less common and often associated with underlying brain abnormalities or systemic conditions:
Brain malformations (e.g., cortical dysplasia)
Metabolic disorders (e.g., hypoglycemia, mitochondrial diseases)
Neurodegenerative diseases
Head trauma (rarely)
Infections affecting the CNS (e.g., encephalitis)
Toxic exposures or withdrawal from certain drugs
3. Triggers (Not true causes, but can provoke seizures)
Hyperventilation
Flashing lights (photosensitivity)
Stress or emotional disturbances
Lack of sleep
Skipping medications
Symptoms
-Core Symptoms
Sudden, brief lapse in awareness (usually 5–20 seconds)
Staring blankly or “zoning out”
Unresponsive during the episode
Abrupt onset and termination – no warning and no post-ictal confusion
No memory of the event afterward
-Associated Features (in some cases)
Automatisms (involuntary repetitive movements)
Lip smacking
Eye blinking or fluttering
Chewing motions
Finger rubbing or hand movements
Mild facial twitching
Mild reduction in muscle tone (but not enough to cause collapse)
Speech interruption if the patient is talking
-Frequency and Duration
Can occur dozens to hundreds of times per day
Each episode usually lasts 5–20 seconds
-Important Notes
The child usually resumes activity immediately after the seizure
No aura before the seizure
No confusion or fatigue afterward
Often first noticed by teachers or parents due to poor attention in class
Types of Absence Seizures
1. Typical Absence Seizures
Most common form, especially in children
Sudden onset and sudden end
Lasts about 5 to 20 seconds
Characterized by:
Brief loss of awareness or staring spells
Minimal or no motor symptoms (may have subtle automatisms like eye blinking or lip-smacking)
EEG shows generalized 3 Hz spike-and-wave discharges
Often triggered by hyperventilation
Usually part of Childhood Absence Epilepsy (CAE)
Generally respond well to treatment and have a good prognosis
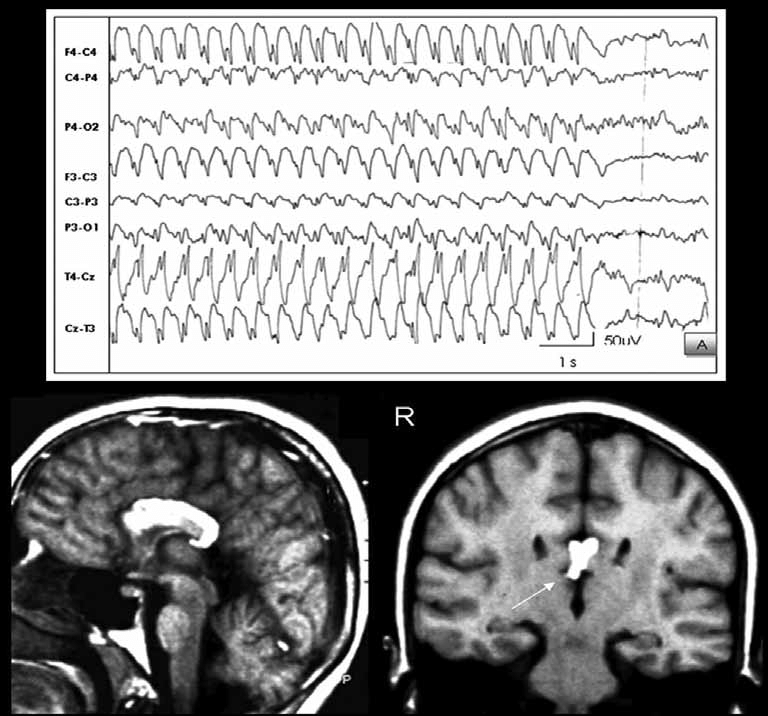
2. Atypical Absence Seizures
Less common; usually seen in patients with developmental delay or other neurological abnormalities
Gradual onset and offset, lasting longer than typical absence seizures (up to several seconds or minutes)
More pronounced motor symptoms such as:
Slower impairment of consciousness
Changes in muscle tone (e.g., mild jerking or tonic posturing)
EEG shows slower (<2.5 Hz) and irregular spike-and-wave complexes
Often associated with syndromes such as Lennox-Gastaut syndrome
More resistant to treatment and poorer prognosis
Investigations & Lab Results
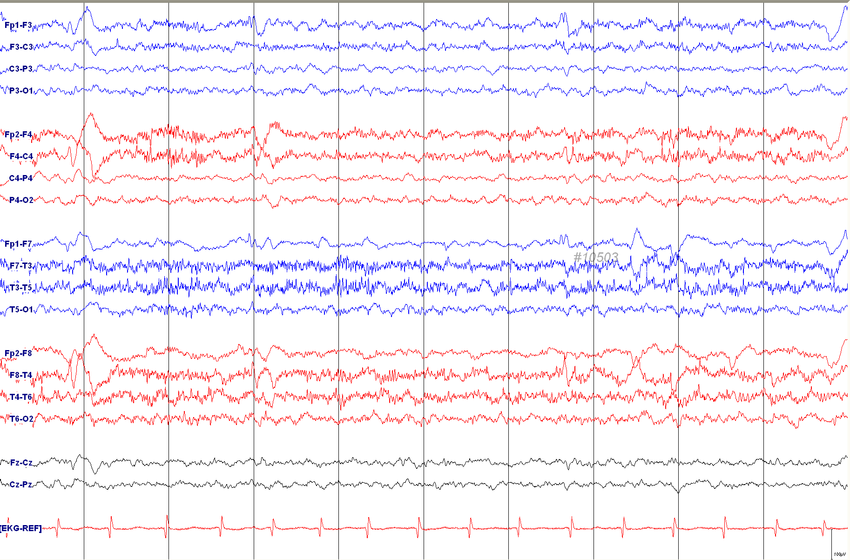
1. Electroencephalogram (EEG) – Most important test
Classic finding: generalized 3 Hz spike-and-wave discharges
These discharges are symmetrical and synchronous across both hemispheres
May be provoked by hyperventilation during EEG
Atypical absence seizures may show slower (<2.5 Hz) spike-and-wave activity
EEG is both diagnostic and specific for absence seizures
2. Hyperventilation Provocation Test
Performed during EEG to induce seizure activity
Hyperventilation for 3–5 minutes can provoke an absence seizure in susceptible individuals
Helps confirm the diagnosis in unclear cases
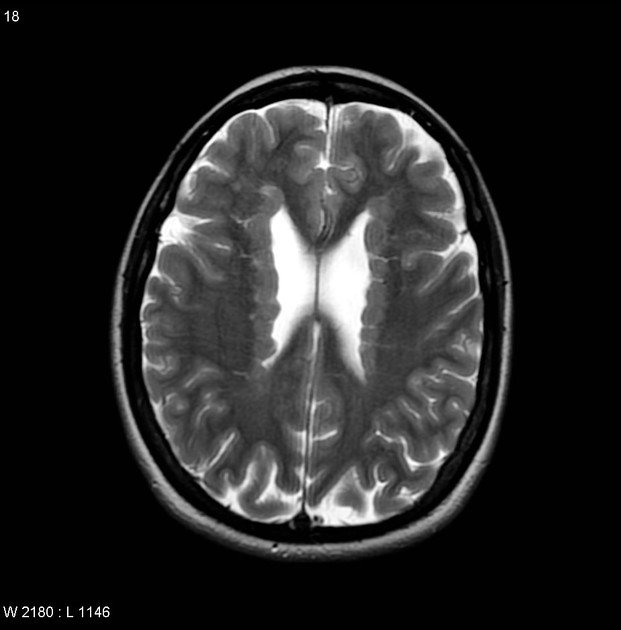
3. Neuroimaging (MRI or CT Brain)
Usually normal in typical absence seizures
Indicated only if:
Atypical features are present
Focal neurological signs or developmental delays exist
Seizures are refractory to treatment
4. Routine Blood Tests
Not diagnostic, but may be done to rule out secondary causes:
Glucose (to exclude hypoglycemia)
Electrolytes (to exclude metabolic causes)
Calcium and magnesium (if metabolic seizures are suspected)
5. Genetic Testing (rarely done)
May be considered in cases with a family history or suspected genetic epilepsy syndrome
Complications
1. Academic and Behavioral Issues
Frequent seizures (dozens to hundreds daily) can cause:
Poor concentration
Reduced academic performance
Difficulty in learning and memory
Misdiagnosis as ADHD or behavioral disorders
2. Social and Emotional Effects
Embarrassment or social isolation
Poor self-esteem, especially in older children or teens
Anxiety about having seizures in public or school
3. Safety Risks
Injury from unawareness during activities (e.g., crossing streets, swimming)
Interference with driving in older adolescents or adults
4. Progression to Other Seizure Types
Some patients may later develop:
Generalized tonic-clonic seizures
Juvenile myoclonic epilepsy (JME)
Atypical absence seizures (more resistant to treatment)
5. Treatment Side Effects
Cognitive slowing, weight changes, or GI upset from medications like:
Valproic acid
Ethosuximide
Lamotrigine
6. Refractory Seizures (Rare)
In some cases (especially atypical absence seizures), seizures may be:
Resistant to treatment
Associated with neurodevelopmental syndromes like Lennox-Gastaut
7. Psychosocial Impact on Family
Emotional stress on caregivers
Difficulty managing school and daily life for the child
Treatment
1. First-Line Medications
–Ethosuximide
Drug of choice for typical absence seizures
Especially in Childhood Absence Epilepsy (CAE)
Few cognitive side effects
Not effective for other types of generalized seizures
Side effects: GI upset, drowsiness, headache
-Valproic Acid (Valproate)
Used when:
Patient has absence + generalized tonic-clonic seizures
Ethosuximide is not effective or not tolerated
Broad-spectrum antiepileptic
Side effects: weight gain, tremor, liver toxicity, teratogenicity (avoid in females of childbearing age unless necessary)
-Lamotrigine
Alternative if ethosuximide and valproate are not suitable
Fewer side effects but less effective
Side effects: rash (including rare SJS), dizziness
2. Other Treatment Options (in refractory or atypical cases)
Clobazam or Topiramate (less commonly used)
Ketogenic diet (in medically refractory epilepsy)
Surgical evaluation if seizures are resistant and another pathology is suspected (rare for pure absence seizures)
3. Supportive Management
Patient and family education
Avoid triggers: sleep deprivation, hyperventilation, stress, flashing lights
School support: address attention, memory, and performance issues
Regular follow-up and EEG monitoring
Prognosis
The prognosis of absence seizures depends on whether the seizures are typical or atypical, as well as the presence of other neurological or developmental conditions.
-Typical Absence Seizures
Generally favorable prognosis
Commonly associated with Childhood Absence Epilepsy (CAE)
Seizures often begin between ages 4 and 10
65–80% of children become seizure-free during adolescence
Normal cognitive development in most cases if well treated
Low risk of developing other seizure types
-Atypical Absence Seizures
Seen in more complex epilepsy syndromes like Lennox-Gastaut syndrome
Poorer prognosis
Often associated with:
Developmental delays
Cognitive impairment
Other seizure types (e.g., atonic, tonic, myoclonic)
More likely to be refractory to treatment
-Factors Indicating Good Prognosis
Early diagnosis and treatment
Good response to first-line anti-seizure medications
No other seizure types
Normal neurological development
Normal EEG background activity between seizures
-Factors Indicating Poor Prognosis
Atypical EEG patterns (e.g., slow spike-and-wave)
Coexisting seizure types
Developmental or intellectual impairment
Resistance to multiple anti-epileptic drugs