Scaphoid Fracture
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
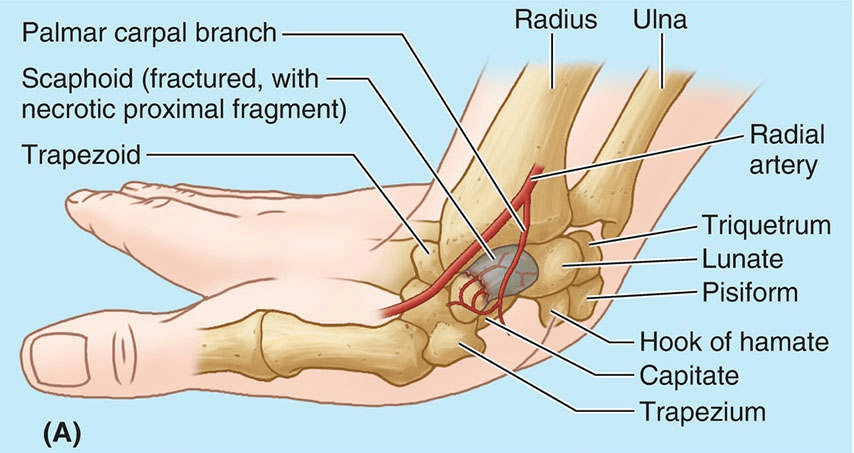
Anatomical Overview
The scaphoid is the most frequently fractured carpal bone. It often results from a fall on the palm when the hand is abducted, the fracture occurring across the narrow part of the scaphoid. On palpation, pain is produced in the anatomical snuff box on the lateral side of the wrist, especially during dorsiflexion and abduction of the hand. Initial radiographs of the wrist may not reveal a fracture; often, this injury is (mis)diagnosed as a severely sprained wrist.

Causes
Fall onto an Outstretched Hand (FOOSH): This is the most common mechanism of injury for scaphoid fractures. When someone falls onto their outstretched hand, the force can be transmitted up the arm, causing the scaphoid bone to bear a significant amount of stress, leading to fracture.
Sports Injuries: Activities such as skiing, snowboarding, skateboarding, and contact sports increase the risk of scaphoid fractures due to the potential for falls or impacts onto the hand or wrist.
Motor Vehicle Accidents: Traumatic incidents such as car accidents can subject the wrist to forces that may result in scaphoid fractures.
Direct Blows to the Wrist: A direct blow to the wrist, such as during a physical altercation or industrial accident, can cause a fracture of the scaphoid bone.
Repetitive Stress: Overuse injuries from repetitive activities that strain the wrist, such as those common in certain occupations (e.g., carpentry, plumbing) or sports (e.g., gymnastics, weightlifting), can lead to stress fractures in the scaphoid over time.
Weak Bones: Individuals with weakened bones due to conditions like osteoporosis are more prone to fractures from minor trauma or falls, including fractures of the scaphoid.
Anatomical Variations: Some individuals may have anatomical variations in the shape or alignment of their scaphoid bone, which can predispose them to fractures under certain circumstances.
Treatment
Immobilization: For stable, non-displaced fractures, immobilization is often the initial treatment. This typically involves wearing a splint or a cast to stabilize the wrist and allow the bone to heal. The duration of immobilization may vary but can range from several weeks to a few months.
Casting: In cases where the fracture is stable but displaced, or if there’s uncertainty about the stability, a cast may be used to maintain proper alignment and support during the healing process. Sometimes, the cast may need to be changed or adjusted based on follow-up imaging.
Surgery: Surgery may be necessary for certain types of scaphoid fractures, such as those that are displaced, unstable, or non-healing (nonunion). Surgical options include:
- Open Reduction Internal Fixation (ORIF): In this procedure, the surgeon realigns the fractured pieces of the scaphoid bone and secures them in place using screws, wires, or plates.
- Percutaneous Screw Fixation: A minimally invasive technique where screws are inserted through small incisions to stabilize the fracture fragments.
- Bone Grafting: In cases of nonunion where the bone fails to heal, bone grafts may be used to promote healing and stimulate bone growth.
Follow-up Care: Regardless of the treatment approach, regular follow-up appointments with a healthcare professional are important to monitor the healing progress, adjust treatment as needed, and assess for any complications.
Physical Therapy: After the immobilization period or surgical intervention, physical therapy may be recommended to improve wrist strength, range of motion, and function. These exercises help to restore normal wrist movement and prevent stiffness.
Activity Modification: During the healing process, it’s essential to avoid activities that may stress the wrist or increase the risk of re-injury. Gradual return to normal activities should be guided by the healthcare provider’s recommendations.