Myocardial Infarction (Heart Attack)
Content of This Page
Introduction
1- Introduction
2- Causes
3- Pathophysiology
4- Signs & Symptoms
5- Risk Factors
6- ECG Changes
7- Investigations & Lab Results
8- Complications
9- Treatment
Causes
Atherosclerotic plaque rupture or erosion (most common cause)
Coronary artery thrombosis (blood clot formation)
Coronary artery spasm (transient narrowing of the artery)
Severe coronary artery narrowing due to stable atherosclerosis
Imbalance between oxygen supply and demand :
Severe anaemia
Hypotension or shock
Sepsis
Tachyarrhythmias (e.g., atrial fibrillation)
Severe hypertension with or without left ventricular hypertrophy
Coronary artery dissection (tear in the artery wall)
Drug-induced vasospasm (e.g., cocaine, amphetamines)
Embolism to the coronary arteries (rare)
Pathophysiology
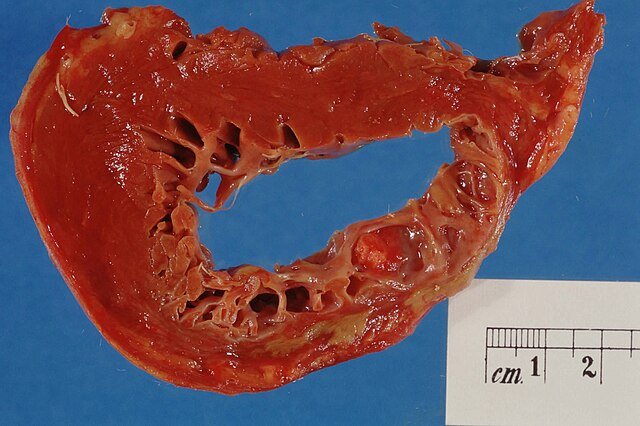
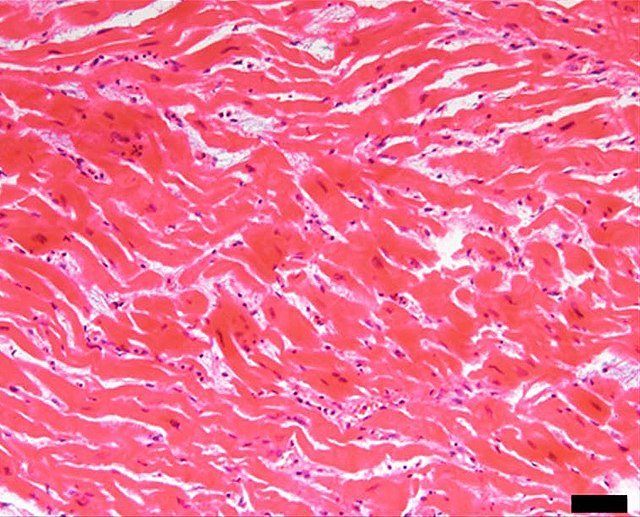
Atherosclerotic plaque rupture or erosion → exposure of subendothelial collagen and lipid core → platelet adhesion, activation, and aggregation → formation of a thrombus (blood clot) → partial or complete blockage of a coronary artery → reduced blood flow to the myocardium (ischaemia) → shift to anaerobic metabolism and depletion of ATP → accumulation of lactate and hydrogen ions causing cellular injury → if the blockage persists beyond 20-30 minutes → irreversible myocardial cell death (necrosis) begins → necrosis spreads from the subendocardium to the epicardium over several hours if not treated. the necrotic myocardium triggers inflammation and subsequent healing with scar formation.
Signs & Symptoms
Central chest pain (pressure, tightness, heaviness)
Pain radiating to left arm, jaw, neck, back
Pain duration >20 minutes
Not relieved by rest or nitroglycerin
Dyspnea (shortness of breath)
Diaphoresis (sweating)
Nausea and vomiting
Anxiety or a feeling of impending doom
Palpitations
Syncope or dizziness
Fatigue (especially in women, elderly, diabetics)
Atypical presentations (epigastric pain, indigestion-like symptoms)

Risk Factors
Smoking
Hypertension
Diabetes mellitus
Hyperlipidemia (high LDL, low HDL)
Obesity
Sedentary lifestyle
Family history of premature coronary artery disease
Age (men >45 years, women >55 years)
Male sex
Stress and psychosocial factors
Excessive alcohol consumption
Chronic kidney disease
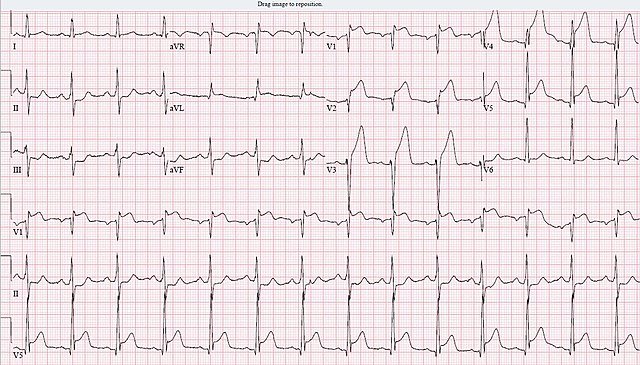
ECG Changes
ST-segment elevation (STEMI)
ST-segment depression (NSTEMI/Ischemia)
T-wave inversion
Pathological Q waves (indicate transmural infarction)
Hyperacute (peaked) T waves (early MI)
New left bundle branch block (LBBB)
Poor R wave progression
Arrhythmias (e.g., ventricular tachycardia, fibrillation)
Complications
Arrhythmias (ventricular tachycardia, ventricular fibrillation)
Cardiogenic shock
Heart failure
Acute mitral regurgitation (papillary muscle rupture)
Ventricular septal rupture
Left ventricular free wall rupture → cardiac tamponade
Pericarditis (early or Dressler’s syndrome)
Left ventricular aneurysm
Thromboembolism (stroke, peripheral embolism)
Re-infarction
Dressler’s syndrome (post-MI pericarditis)
Investigations & Lab Results
-ECG
ST-segment elevation (STEMI)
ST-segment depression (NSTEMI/Ischemia)
T-wave inversion
Pathological Q waves (late finding)
-Cardiac Biomarkers
Troponin I/T – elevated (most sensitive and specific, rises within 3–6 hours)
CK-MB – elevated (useful for detecting reinfarction, rises within 3–6 hours)
Myoglobin – rises early but non-specific
-Blood Tests
Complete blood count (CBC) – may show leukocytosis
Renal function tests – for contrast use and overall assessment
Lipid profile – should be taken early (within 24 hours)
Blood glucose – often elevated in stress or diabetes
-Imaging
Chest X-ray – to exclude other causes (e.g., pneumothorax, heart failure)
Echocardiography – wall motion abnormalities, ejection fraction, complications
Coronary angiography – definitive for locating coronary artery blockages
-Other Tests
D-dimer – to rule out pulmonary embolism if indicated
BNP or NT-proBNP – assess for heart failure if suspected
Treatment
1. Initial Stabilization (MONA)
Morphine — for pain relief and anxiety
Oxygen — if O₂ saturation <90% or respiratory distress
Nitrates — to reduce preload and relieve chest pain (avoid if hypotension)
Aspirin — antiplatelet, chewable, immediately
2. Adjunct Medications
Beta-blockers — reduce myocardial oxygen demand, decrease arrhythmias (avoid in shock, bradycardia)
P2Y12 inhibitors — clopidogrel, ticagrelor, prasugrel to prevent platelet aggregation
Anticoagulants — unfractionated heparin or low molecular weight heparin
Statins — high intensity for plaque stabilization and lipid lowering
ACE inhibitors / ARBs — reduce remodeling and improve survival (especially with LV dysfunction, HTN)
3. Reperfusion Therapy
Primary PCI (Percutaneous Coronary Intervention) — preferred if within 90–120 minutes of first medical contact
Thrombolysis (Fibrinolytics) — if PCI unavailable within recommended timeframe
Coronary artery bypass grafting (CABG) — in multi-vessel disease or failed PCI
4. Management of Complications
Arrhythmias — antiarrhythmics, defibrillation if needed
Heart failure — diuretics, inotropes
Cardiogenic shock — inotropes, mechanical support if necessary
5. Secondary Prevention and Rehabilitation
Smoking cessation
Diet and exercise counseling
Control of diabetes, hypertension, lipids
Cardiac rehabilitation programs