Liver Cirrhosis
content of this page
1- Introduction
2- Anatomical Overview
3- Treatment
4- purposes
Introduction
Liver cirrhosis is a chronic liver condition characterized by scarring of the liver tissue. This scarring, which replaces healthy liver tissue, disrupts the liver’s normal structure and function. Liver cirrhosis is often the result of long-term liver damage and can lead to serious complications, including liver failure. Common causes of liver cirrhosis include chronic alcohol abuse, viral hepatitis, and fatty liver disease.
Anatomical Overview
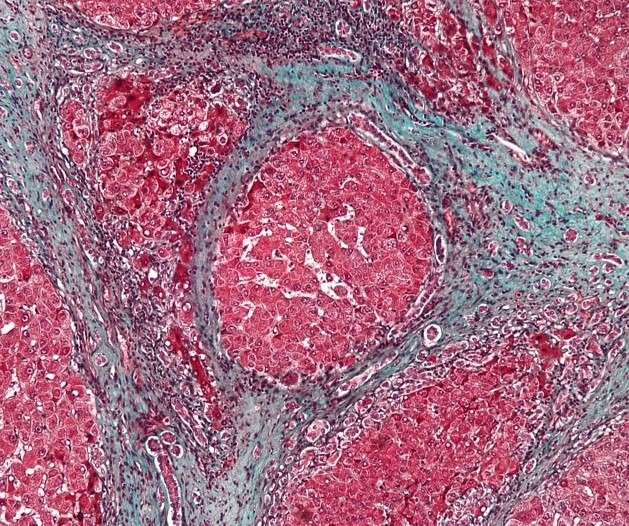
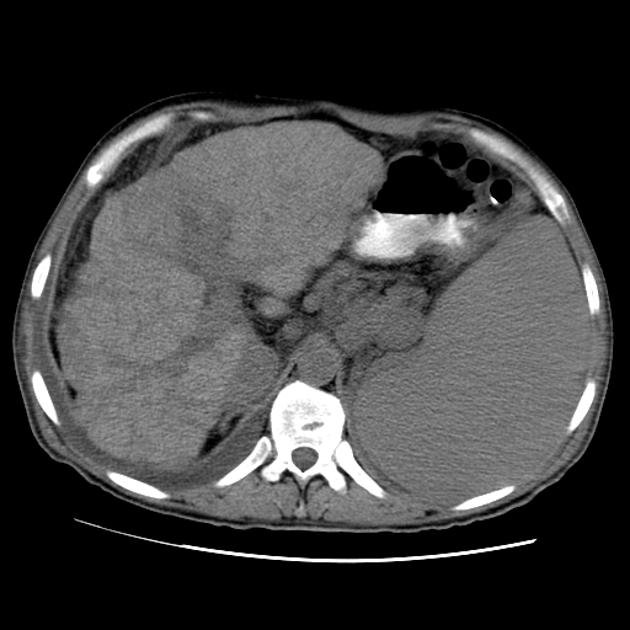
As cirrhosis progresses, fibrous tissue forms septa that divide the liver into nodules of varying sizes. This nodular transformation gives the liver a lumpy appearance and alters its blood flow. The liver’s normal dual blood supply, from the hepatic artery and portal vein, becomes distorted, leading to changes in blood flow patterns and increased resistance to blood flow.
The disruption of normal liver architecture in cirrhosis also affects the liver’s bile ducts. Bile produced by hepatocytes drains into small bile ducts, which eventually merge to form larger bile ducts that carry bile out of the liver. In cirrhosis, fibrous tissue can compress and distort these bile ducts, leading to impaired bile flow and the accumulation of bile within the liver. This can contribute to further liver damage and dysfunction.
The anatomical changes in liver cirrhosis not only affect the liver’s structure but also its function. The liver plays a crucial role in metabolism, detoxification, and the production of proteins and clotting factors. In cirrhosis, these functions can be impaired, leading to complications such as jaundice (yellowing of the skin and eyes), coagulopathy (bleeding disorders), and hepatic encephalopathy (brain dysfunction due to liver failure).
Treatment
Management of Underlying Cause: If cirrhosis is caused by conditions such as chronic viral hepatitis, alcohol abuse, or fatty liver disease, addressing these underlying causes is crucial. This may involve antiviral medications for hepatitis, alcohol cessation programs, and lifestyle changes for fatty liver disease.
Symptom Management: Medications may be prescribed to manage symptoms such as fatigue, itching, and abdominal discomfort. Diuretics may be used to reduce fluid buildup (ascites) and swelling (edema).
Nutritional Support: A balanced diet, low in sodium and protein, may be recommended to reduce the risk of complications and support liver function.
Monitoring and Screening: Regular monitoring of liver function, imaging studies, and screening for complications such as liver cancer are important.
Complications Management: Treatment for complications such as variceal bleeding, hepatic encephalopathy, or ascites may be necessary. This can include medications, procedures (like banding of varices), or in severe cases, liver transplantation.
Lifestyle Changes: Avoiding alcohol, maintaining a healthy weight, and exercising regularly can help slow the progression of cirrhosis and improve overall health.
Liver Transplantation: In severe cases of cirrhosis with liver failure, liver transplantation may be considered. This involves replacing the diseased liver with a healthy liver from a donor.
Purposes
Symptom Management: Many individuals with liver cirrhosis experience symptoms such as fatigue, itching, abdominal discomfort, and nausea. Treatment aims to alleviate these symptoms to improve the patient’s comfort and quality of life.
Slowing Disease Progression: Liver cirrhosis is a progressive condition, meaning it worsens over time. Treatment strategies, such as addressing underlying causes and lifestyle changes, aim to slow down the progression of the disease and preserve liver function for as long as possible.
Preventing Complications: Cirrhosis can lead to serious complications such as ascites (fluid buildup in the abdomen), variceal bleeding (bleeding from enlarged veins in the esophagus or stomach), hepatic encephalopathy (brain dysfunction due to liver failure), and hepatorenal syndrome (kidney failure due to liver dysfunction). Treatment aims to prevent or manage these complications to improve outcomes.
Addressing Underlying Causes: Identifying and treating the underlying causes of liver cirrhosis, such as chronic viral hepatitis, alcohol abuse, or fatty liver disease, is essential. This can involve antiviral medications, alcohol cessation programs, or lifestyle changes to manage these conditions and reduce further liver damage.
Liver Regeneration and Function: While the liver has a remarkable ability to regenerate, this capacity is limited in cirrhosis due to the extensive scarring. Treatment aims to support liver function and promote any remaining regenerative capacity to maintain liver health