Epistaxis
content of this page
1- Introduction
2- Anatomical Overview
3- Causes
4- Treatment
Introduction
Epistaxis, commonly known as a nosebleed, is a common medical condition characterized by bleeding from the nasal passages. It can range from minor, self-limiting episodes to more severe bleeding that requires medical intervention. Epistaxis occurs when the delicate blood vessels lining the nose become damaged or ruptured, leading to bleeding that may originate from either the anterior (front) or posterior (back) parts of the nasal cavity.
Anatomical Overview
Epistaxis (nosebleed) is relatively common because of the rich blood supply to the nasal mucosa. In most cases, the cause of nosebleed is trauma and the bleeding is from an area in the anterior third of the nose (Kiesselbach area). Epistaxis is also associated with infections and hypertension. Spurting of blood from the nose results from rupture of arteries. Mild epistaxis may also result from nose picking, which tears veins in the vestibule of the nose.

Causes
Trauma: Injury to the nose, such as from picking the nose, inserting foreign objects, or blunt trauma (e.g., a blow to the face), can cause blood vessels in the nasal cavity to rupture and bleed.
Dry Air: Dry and heated indoor environments, particularly during winter months or in arid climates, can dry out the nasal mucosa, making blood vessels more prone to rupture.
Nasal Irritation: Irritants like chemicals (e.g., nasal sprays, cocaine use), pollutants, smoke, or strong odors can irritate the nasal passages and lead to epistaxis.
Nasal Fractures or Deformities: Structural abnormalities or deformities of the nose, such as septal deviations or nasal polyps, can disrupt normal blood flow and predispose to nosebleeds.
Medical Conditions:
- Hypertension: High blood pressure can increase the risk of epistaxis, especially if poorly controlled.
- Blood Clotting Disorders: Conditions such as hemophilia, thrombocytopenia (low platelet count), or use of anticoagulant medications (e.g., aspirin, warfarin) can impair blood clotting and increase bleeding tendencies.
- Nasal Infections: Sinusitis or other infections affecting the nasal mucosa can cause inflammation and bleeding.
- Nasal Tumors: Benign or malignant growths in the nasal cavity or sinuses may erode blood vessels and cause bleeding.
- Hereditary Hemorrhagic Telangiectasia (HHT): A genetic disorder that causes abnormal blood vessel formation can lead to recurrent nosebleeds.
Systemic Factors: Conditions that increase blood flow to the nose, such as strenuous physical activity, pregnancy, or alcohol consumption, can predispose to epistaxis.
Medications: Certain medications, such as nasal corticosteroids, nasal decongestants (if used excessively), or medications that affect blood clotting, can contribute to nasal dryness or bleeding.
Environmental Factors: High altitudes or changes in atmospheric pressure (e.g., during air travel) can affect nasal blood vessels and increase the likelihood of nosebleeds.
Treatment
Initial Management (First Aid):
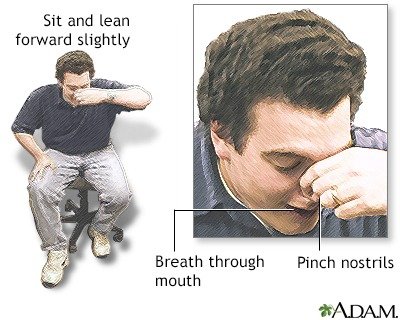
Positioning: Have the person sit upright and lean forward to prevent blood from flowing down the throat, which can cause nausea or choking.
Pinching the Nose: Pinch the soft part of the nose (the nostrils) together with gentle pressure using the thumb and index finger for at least 10-15 minutes. This helps compress the blood vessels and stop the bleeding.
Avoiding Irritants: Advise the person to avoid blowing their nose, vigorous activity, or inserting anything into the nose immediately after a nosebleed.
Medical Interventions:
Nasal Packing: If simple pressure does not stop the bleeding, nasal packing may be required. This involves inserting absorbent material (packing) into the nasal cavity to apply direct pressure on the bleeding site. Packing may be temporary (e.g., with gauze) or involve specialized balloon devices (e.g., nasal tampons).
Cauterization: Chemical cautery or electrical cauterization may be used to seal off bleeding blood vessels. This procedure is typically performed under local anesthesia by a healthcare provider.
Topical Medications: Nasal sprays or gels containing vasoconstrictors (e.g., oxymetazoline) may help constrict blood vessels and control bleeding.
Management of Recurrent or Severe Epistaxis:
Evaluation for Underlying Causes: If nosebleeds are frequent or severe, further evaluation may be necessary to identify and address underlying factors such as nasal trauma, structural abnormalities, hypertension, blood clotting disorders, or nasal tumors.
Surgical Interventions: In some cases, surgical procedures may be recommended for persistent or recurrent epistaxis. This may include cauterization under endoscopic guidance, surgical repair of nasal septal deviations, or ligation of abnormal blood vessels.
Management of Underlying Conditions: Treating underlying medical conditions, such as hypertension or blood clotting disorders, can help reduce the risk of recurrent nosebleeds.
Preventive Measures:
Humidification: Using a humidifier to add moisture to indoor air can help prevent nasal dryness and reduce the risk of nosebleeds, especially in dry climates or during winter months.
Nasal Lubrication: Applying a thin layer of saline nasal gel or ointment inside the nostrils can help keep the nasal mucosa moist and reduce irritation.
Avoiding Nasal Trauma: Encouraging gentle nose blowing and avoiding picking the nose can minimize the risk of trauma to nasal blood vessels.
When to Seek Medical Attention:
- If nosebleeds are frequent, severe, or prolonged (lasting more than 20-30 minutes despite initial measures).
- If there is significant bleeding after an injury to the head or face.
- If nosebleeds occur in individuals with a history of bleeding disorders or use of blood-thinning medications.