Spinal Cord Injury
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
A spinal cord injury (SCI) refers to damage or trauma to the spinal cord resulting in a loss of function, often affecting movement, sensation, and bodily functions below the level of the injury. These injuries can vary widely in severity and location along the spine, leading to diverse degrees of impairment. Spinal cord injuries can result from accidents, falls, sports injuries, or medical conditions, and they require immediate medical attention to assess and stabilize the injury. Treatment and rehabilitation focus on minimizing complications, restoring function, and improving quality of life for individuals affected by these injuries.
Pathophysiology
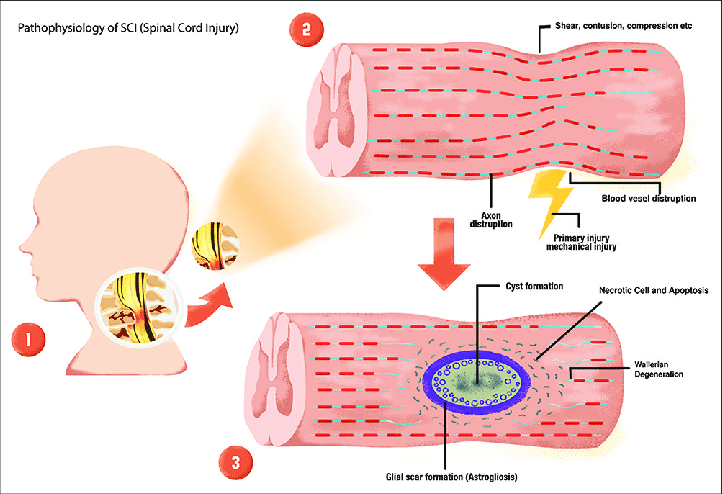
A spinal cord injury (SCI) disrupts the normal functioning of the spinal cord, which is a crucial component of the central nervous system responsible for transmitting signals between the brain and the rest of the body. When the spinal cord is injured, the communication pathway between the brain and the body below the injury site is interrupted. The severity and extent of impairment depend on the location and severity of the injury along the spinal cord.
Physiologically, an SCI can lead to immediate and profound changes in motor, sensory, and autonomic functions. Motor function refers to movement and control of muscles, and injuries can result in partial or complete paralysis (paraplegia or quadriplegia). Sensory function involves the ability to feel and perceive sensations such as touch, temperature, and pain. Damage to sensory pathways can lead to loss of sensation or abnormal sensations below the level of injury. Autonomic functions, which include blood pressure regulation, bladder and bowel control, and sexual function, may also be affected, often resulting in disruptions that require management.
In the acute phase of SCI, there is often swelling and inflammation around the injury site, which can further damage nerve cells and worsen functional impairment. Depending on the severity, SCI can lead to lifelong disability, impacting an individual’s independence and quality of life. Rehabilitation plays a crucial role in maximizing recovery and adaptation to functional changes. This may include physical therapy to strengthen muscles, improve mobility, and prevent complications such as muscle contractures or pressure sores.

Symptoms
Loss of Movement (Paralysis):
- SCI can result in partial or complete loss of movement (paralysis) below the level of the injury. Paralysis may affect one or both sides of the body (hemiplegia) and can be categorized as paraplegia (lower body paralysis) or quadriplegia/tetraplegia (paralysis of all four limbs).
Loss of Sensation:
- Damage to sensory nerves can lead to loss of sensation below the level of the injury. Individuals may experience reduced ability to feel touch, temperature changes, or pain in affected areas.
Changes in Bowel and Bladder Function:
- SCI can disrupt the nerves that control bowel and bladder function, leading to difficulty in controlling these functions. This may result in incontinence (involuntary leakage) or difficulty emptying the bladder or bowels.
Impaired Breathing:
- Injuries at higher levels of the spinal cord (cervical or upper thoracic) can affect the muscles involved in breathing, potentially requiring assistance with breathing (ventilation) depending on the extent of the injury.
Spasticity or Muscle Stiffness:
- Damage to nerve pathways can lead to increased muscle tone and spasms (spasticity), which may cause stiffness or uncontrollable muscle contractions in affected limbs.
Loss of Sexual Function:
- SCI can affect sexual arousal, sensation, and function due to disruptions in nerve signals controlling sexual responses.
Changes in Blood Pressure and Heart Rate:
- Autonomic dysreflexia, a potentially dangerous condition characterized by sudden high blood pressure, sweating, and headache, can occur in individuals with SCI, particularly in injuries above the T6 level.
Chronic Pain:
- Some individuals may experience chronic pain, including neuropathic pain (nerve-related pain) or musculoskeletal pain, at or near the site of the injury.
Secondary Complications:
- Individuals with SCI are at increased risk for secondary complications such as pressure ulcers (bedsores), urinary tract infections, pneumonia, deep vein thrombosis (DVT), and osteoporosis due to reduced mobility and altered body function.
Treatment
Surgery: Surgical removal of the pituitary tumor (transsphenoidal surgery) is often the first-line treatment if the tumor is accessible and the individual is in good health. Successful surgery can lead to rapid normalization of GH and IGF-1 levels. In some cases, additional treatment may be needed if the tumor cannot be completely removed.
Medications:
- Somatostatin analogs (SSAs): Drugs like octreotide and lanreotide can reduce GH secretion and lower IGF-1 levels. These are typically used if surgery is not fully successful or as a pre-operative treatment to shrink the tumor.
- Dopamine agonists: Drugs like cabergoline can sometimes be used to lower GH levels, particularly in cases where the tumor also secretes prolactin.
- Growth hormone receptor antagonists: Pegvisomant is an injectable medication that blocks the action of GH and lowers IGF-1 levels. It is used in cases where other treatments are not effective.
Radiation therapy: This may be considered if the tumor persists or recurs after surgery and is not responsive to medications. Radiation therapy aims to shrink or destroy the tumor cells over time.
Monitoring and management: Regular follow-up with healthcare providers is essential to monitor hormone levels, assess tumor growth, and manage any ongoing symptoms or complications. This may involve adjustments to medications or additional treatments as needed.
Lifestyle considerations: Managing symptoms such as joint pain, sleep apnea, and cardiovascular risks through lifestyle changes, physical therapy, and appropriate medical interventions can help improve quality of life.