Irritable Bowel Syndrome
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
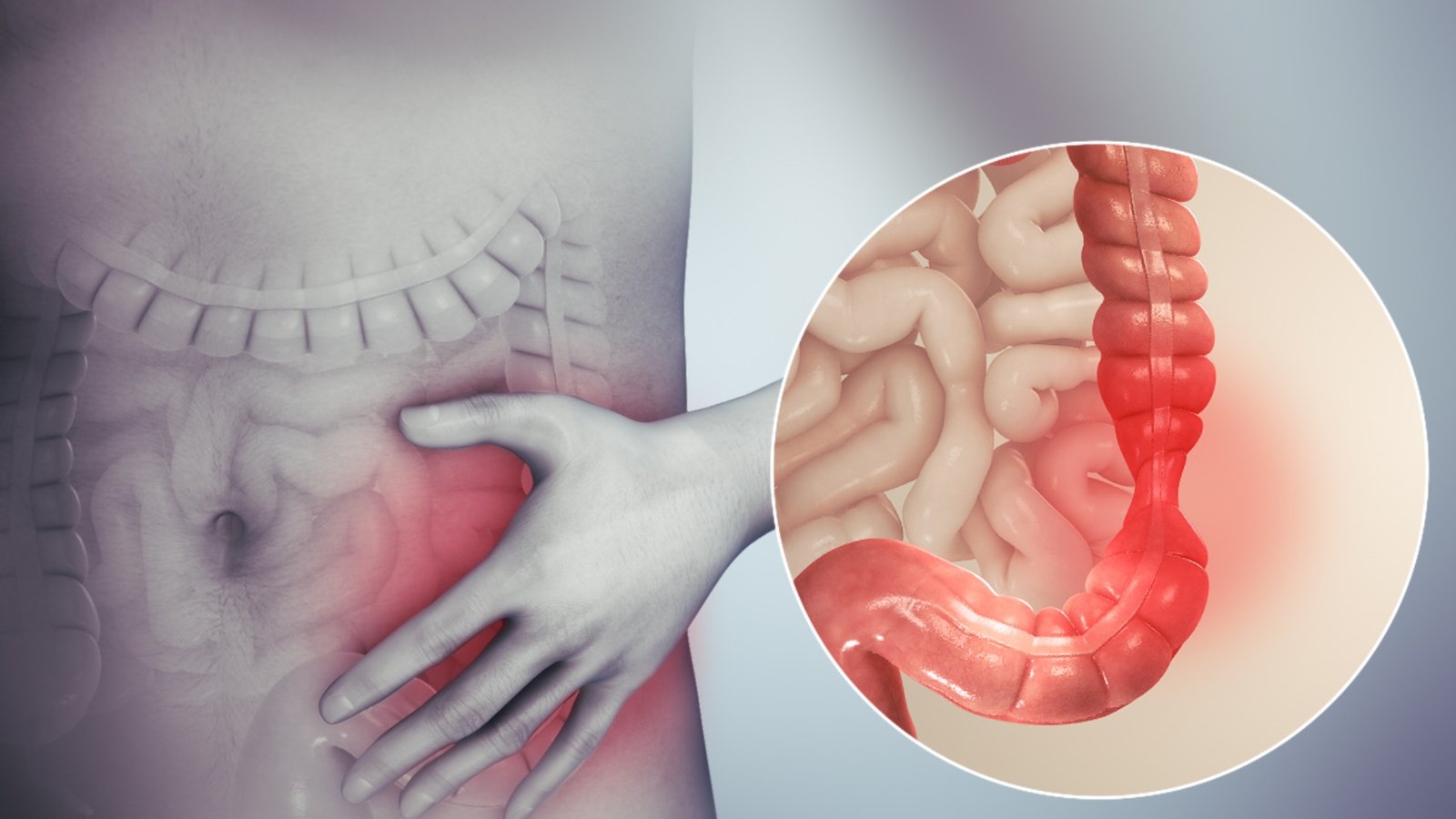
Irritable Bowel Syndrome (IBS) is a common gastrointestinal disorder characterized by a combination of symptoms that can include abdominal pain, cramping, bloating, and changes in bowel habits such as diarrhea, constipation, or both. Unlike inflammatory bowel diseases like Crohn’s disease or ulcerative colitis, IBS does not cause permanent damage to the intestines or increase the risk of colorectal cancer. The exact cause of IBS is not fully understood, but it is believed to involve a combination of factors such as abnormal gastrointestinal motility, heightened sensitivity to intestinal pain, changes in gut microbiota, and psychological factors such as stress or anxiety. Management typically involves dietary changes, lifestyle modifications, stress management techniques, and sometimes medications to alleviate symptoms and improve quality of life.
Pathophysiology
The pathophysiology of Irritable Bowel Syndrome (IBS) involves a complex interplay of factors affecting the gastrointestinal tract, nervous system, and psychological well-being. Central to IBS is the dysregulation of gastrointestinal motility, characterized by abnormal contractions of the intestinal muscles. This dysmotility can lead to the hallmark symptoms of IBS, including diarrhea, constipation, or alternating bouts of both. Individuals with IBS often exhibit visceral hypersensitivity, meaning they experience heightened sensitivity to pain and discomfort in the intestines, which can occur at lower thresholds of stimulation.
Beyond these physical manifestations, dysfunction in the brain-gut axis plays a critical role in IBS. This bidirectional communication pathway between the central nervous system and the gut involves intricate signaling mechanisms that regulate intestinal function and sensitivity. In IBS, disturbances in this axis contribute to the perception and processing of pain and discomfort in the gut. Psychological factors such as stress, anxiety, and depression can exacerbate symptoms through this pathway, further complicating the condition.
While IBS is not characterized by overt inflammation like inflammatory bowel diseases (IBD), some studies suggest subtle immune activation and inflammatory changes in the intestinal lining may contribute to symptoms in certain individuals. Additionally, alterations in the gut microbiota, the community of microorganisms residing in the intestines, have been observed in people with IBS. These changes may influence intestinal function, immune response, and the production of gas and other metabolites that can contribute to symptoms.

Symptoms
Abdominal Pain and Discomfort: Often described as cramping, which may vary in intensity and location within the abdomen.
Changes in Bowel Habits:
- Diarrhea: Frequent loose or watery stools.
- Constipation: Infrequent bowel movements or difficulty passing stool.
- Alternating Bowel Habits: Fluctuation between diarrhea and constipation.
Bloating and Gas: Feeling of fullness or distension in the abdomen, often accompanied by increased gas production.
Mucus in Stool: Passage of mucus along with stool, which is a common but non-specific symptom of IBS.
Urgency: Sudden, compelling need to have a bowel movement, which can be difficult to control.
Incomplete Evacuation: Sensation that bowel movements are incomplete or that the rectum hasn’t been emptied entirely.
Fatigue and Sleep Disturbances: Many individuals with IBS experience fatigue, disrupted sleep patterns, or low energy levels, often related to the impact of symptoms on daily life and psychological well-being.
Psychological Symptoms: Stress, anxiety, and depression are commonly associated with IBS and can worsen gastrointestinal symptoms.
Treatment
1. Lifestyle Modifications:
- Stress Management: Techniques such as mindfulness meditation, deep breathing exercises, and yoga can help reduce stress levels, which can exacerbate IBS symptoms.
- Regular Exercise: Physical activity can promote regular bowel function and alleviate symptoms. Aim for at least 30 minutes of moderate exercise most days of the week.
- Adequate Sleep: Getting enough restful sleep can help manage overall well-being and reduce fatigue associated with IBS.
2. Dietary Changes:
- Fiber: Gradually increasing dietary fiber intake, especially soluble fiber found in oats, beans, and fruits like apples and berries, can help regulate bowel movements and alleviate constipation.
- Low-FODMAP Diet: Some individuals with IBS benefit from a temporary low-FODMAP diet, which restricts certain carbohydrates that may contribute to symptoms like bloating and gas. This diet is typically followed under the guidance of a healthcare provider or dietitian.
- Hydration: Drinking plenty of water throughout the day helps maintain hydration and can aid in regular bowel function.
3. Medications:
- Antispasmodics: Medications such as dicyclomine (Bentyl) or hyoscyamine (Levsin) can help reduce abdominal cramping and pain by relaxing the muscles in the intestines.
- Antidiarrheals: Loperamide (Imodium) may be used to control diarrhea, although it is not recommended for long-term use.
- Laxatives: Polyethylene glycol (MiraLAX) or other laxatives may be recommended for individuals with IBS-C to alleviate constipation.
- Tricyclic Antidepressants (TCAs): In low doses, TCAs like amitriptyline can help relieve abdominal pain and improve symptoms, especially in individuals with IBS-D.
4. Psychological Therapies:
- Cognitive Behavioral Therapy (CBT): CBT can help individuals with IBS learn coping strategies for managing stress, anxiety, and symptoms related to their condition.
- Mindfulness-Based Therapies: Mindfulness techniques can help improve overall well-being and reduce the impact of psychological factors on gastrointestinal symptoms.
5. Probiotics:
- Probiotic Supplements: Some evidence suggests that certain probiotics may help alleviate symptoms of IBS, particularly those with a mix of Bifidobacterium and Lactobacillus strains. However, the effectiveness can vary, and it’s important to choose probiotics based on individual symptoms and needs.
6. Education and Support:
- Patient Education: Understanding triggers and management strategies can empower individuals to better manage their symptoms and improve quality of life.
- Support Groups: Joining support groups or seeking peer support can provide emotional support and practical tips for living with IBS.
7. Medical Monitoring:
- Regular Follow-Up: Periodic check-ins with a healthcare provider can help monitor symptoms, adjust treatment as needed, and rule out other potential causes for symptoms.