Peripheral Neuropathy
content of this page
1- Introduction
2- Pathophysiology
3- Symptoms
4- Treatment
Introduction
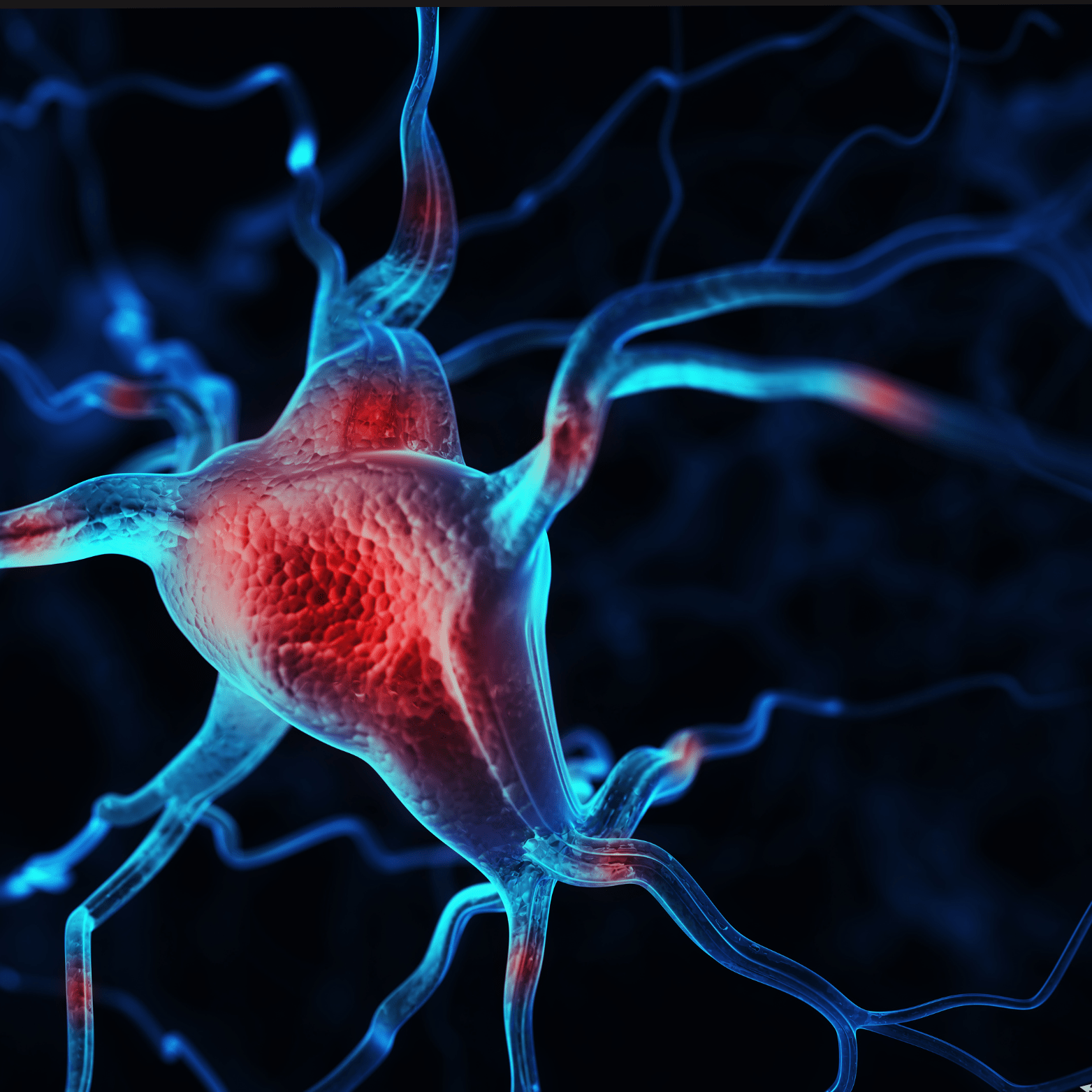
Peripheral neuropathy refers to a condition where nerves outside of the brain and spinal cord (peripheral nerves) are damaged, resulting in a variety of symptoms. These nerves transmit signals between the body, the spinal cord, and the brain, enabling sensation, movement, and other functions. When damaged, they can cause symptoms ranging from numbness and tingling to more severe issues like muscle weakness or difficulty coordinating movements. Many conditions can cause peripheral neuropathy, including diabetes, infections, autoimmune diseases, and certain medications or toxins.
Pathophysiology
Peripheral neuropathy encompasses a diverse array of conditions characterized by damage to the peripheral nerves, disrupting their ability to transmit signals between the central nervous system (CNS) and the body. The pathophysiology involves several underlying mechanisms that can lead to nerve dysfunction and injury. One primary mechanism is axonal degeneration, where the nerve fibers (axons) themselves undergo damage, disrupting signal transmission. This can occur due to direct physical trauma, metabolic disorders such as diabetes mellitus which leads to chronic hyperglycemia and nerve damage, or through autoimmune responses where the immune system mistakenly attacks the peripheral nerves, as seen in conditions like Guillain-Barré syndrome or chronic inflammatory demyelinating polyneuropathy (CIDP). Additionally, demyelination, where the protective myelin sheath surrounding nerve fibers is damaged or destroyed, can occur. This slows down or blocks nerve conduction, leading to symptoms such as sensory disturbances, weakness, and loss of motor control. Various factors including infections (e.g., HIV, Lyme disease), exposure to toxins (e.g., chemotherapy drugs, heavy metals), and genetic predispositions can contribute to peripheral neuropathy by triggering these pathological processes.

Symptoms
Sensory Symptoms:
- Numbness or Tingling: Often described as “pins and needles” sensations in the hands or feet.
- Burning or Shooting Pain: Sharp, stabbing pain or a burning sensation, which can be persistent or intermittent.
- Hypersensitivity: Heightened sensitivity to touch, temperature changes, or pressure.
- Loss of Coordination: Difficulty with fine motor tasks, such as buttoning clothes or picking up objects.
Motor Symptoms:
- Muscle Weakness: Difficulty moving muscles, particularly in the hands or feet.
- Muscle Twitching or Cramping: Involuntary muscle contractions or spasms.
- Muscle Wasting: Gradual loss of muscle mass due to lack of use or nerve damage.
Autonomic Symptoms:
- Changes in Blood Pressure: Fluctuations in blood pressure, often when moving from sitting to standing (orthostatic hypotension).
- Heart Rate Irregularities: Abnormal heart rate or rhythm due to autonomic nerve dysfunction.
- Digestive Issues: Problems with digestion, including diarrhea, constipation, or difficulty swallowing.
- Bladder Dysfunction: Difficulty emptying the bladder completely (urinary retention) or involuntary loss of urine (urinary incontinence).
Other Symptoms:
- Balance Problems: Difficulty maintaining balance and coordination, leading to an increased risk of falls.
- Temperature Sensitivity: Inability to sense temperature changes, which can lead to burns or other injuries.
- Sexual Dysfunction: Erectile dysfunction in men and difficulty achieving orgasm in both men and women.
Treatment
Medications:
- Pain Management: Over-the-counter pain relievers (such as acetaminophen or nonsteroidal anti-inflammatory drugs) may help relieve mild to moderate pain. For more severe neuropathic pain, medications such as tricyclic antidepressants (e.g., amitriptyline), anticonvulsants (e.g., gabapentin, pregabalin), or serotonin-norepinephrine reuptake inhibitors (SNRIs) like duloxetine may be prescribed.
- Topical Treatments: Topical creams or patches containing capsaicin (derived from chili peppers) or lidocaine can provide localized pain relief.
- Opioid Medications: In severe cases of neuropathic pain that do not respond to other treatments, opioids may be considered, but these are generally used cautiously due to the risk of dependence and side effects.
Physical Therapy and Rehabilitation:
- Exercise: Regular physical activity and exercises prescribed by a physical therapist can help improve muscle strength, coordination, and balance.
- Occupational Therapy: Techniques to adapt daily activities and improve function despite nerve damage.
Treatment of Underlying Conditions:
- Control of Blood Sugar: For individuals with diabetic neuropathy, maintaining tight control of blood glucose levels is crucial to slow the progression of nerve damage.
- Management of Infections: Treating infections that contribute to neuropathy, such as antiviral medications for herpes zoster or antibiotics for bacterial infections.
Lifestyle Modifications:
- Foot Care: Proper foot care is essential to prevent complications such as ulcers and infections in individuals with peripheral neuropathy, especially those with diabetes.
- Pain Management Techniques: Relaxation techniques, biofeedback, and acupuncture may provide additional relief from neuropathic pain.
Nutritional Supplements:
- Vitamin B12: Supplements may be recommended for individuals with deficiencies that contribute to neuropathy.
- Alpha-Lipoic Acid: Antioxidant supplements like alpha-lipoic acid have shown some benefit in reducing symptoms of diabetic neuropathy.
Transcutaneous Electrical Nerve Stimulation (TENS):
- TENS therapy involves applying mild electrical impulses to nerve endings through electrodes placed on the skin. This can help reduce pain and improve nerve function in some individuals.
Surgical Interventions:
- In rare cases where neuropathy is caused by nerve compression (e.g., carpal tunnel syndrome), surgical decompression may be considered to relieve pressure on the affected nerve.
Psychological Support:
- Living with chronic pain and disability from peripheral neuropathy can lead to emotional stress and depression. Counseling or support groups may be beneficial to help cope with the psychological impact of the condition.