Muscle Atrophy
content of this page
1- Introduction
2- Pathophysiology
3- Causes
4- Treatment
Introduction
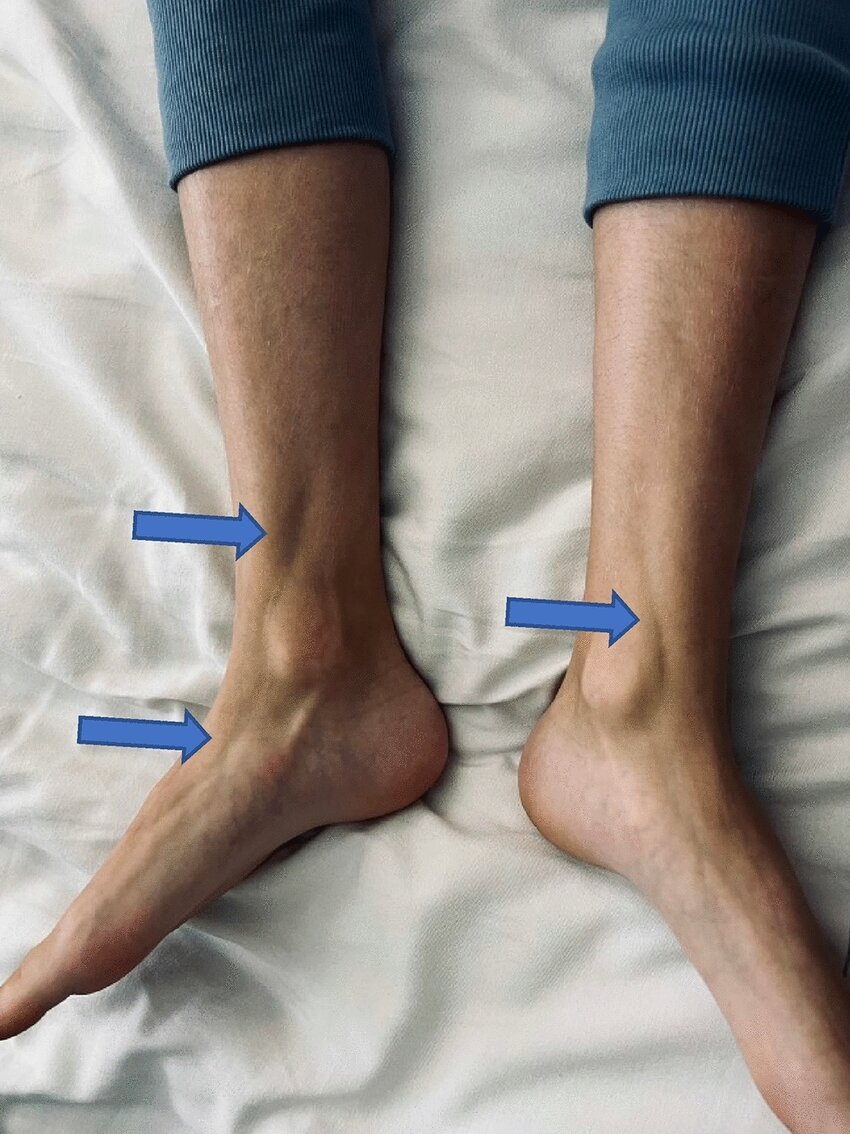
Muscle atrophy, often simply referred to as muscle wasting, is a condition characterized by a decrease in muscle mass and strength. It occurs when muscles weaken and shrink due to various factors, such as lack of physical activity, aging, injury, or certain medical conditions. Muscle atrophy can affect specific muscles or groups of muscles throughout the body, leading to weakness, reduced mobility, and functional impairment.
Pathophysiology
The pathophysiology of muscle atrophy involves a cascade of biological processes that disrupt the normal balance between muscle protein synthesis and breakdown. Disuse or immobilization is a common trigger, where muscles undergo atrophy due to reduced mechanical tension and diminished neural stimulation. This lack of activity leads to a decrease in muscle fiber size and mass over time. Neurological conditions, such as spinal cord injuries or motor neuron diseases, interfere with the communication between nerves and muscles, impairing muscle contraction and leading to progressive weakness and wasting.
At a cellular level, muscle atrophy involves changes in protein metabolism. Normally, muscle fibers constantly adjust their protein content through a dynamic process of synthesis and degradation. During atrophy, there is an increase in protein breakdown pathways, such as the ubiquitin-proteasome system and autophagy, which target muscle proteins for degradation. This heightened breakdown exceeds the rate of protein synthesis, resulting in a net loss of muscle protein and mass.
Inflammatory cytokines, particularly tumor necrosis factor-alpha (TNF-α) and interleukins, play a role in promoting muscle protein breakdown in various chronic diseases and conditions associated with muscle wasting. These cytokines induce muscle fiber apoptosis (cell death) and interfere with muscle regeneration processes. Hormonal changes, such as decreased levels of anabolic hormones like testosterone and growth hormone, further exacerbate muscle atrophy by reducing protein synthesis and promoting protein breakdown.
Moreover, oxidative stress and mitochondrial dysfunction contribute to muscle damage and impaired muscle function, particularly in conditions associated with chronic inflammation or metabolic disorders. Genetic factors can also predispose individuals to certain forms of muscle atrophy, such as muscular dystrophies, where mutations in genes encoding structural proteins compromise muscle integrity and function over time.
Causes
Disuse or Immobilization: When muscles are not used regularly or are immobilized due to injury, illness, or prolonged bed rest, they can undergo disuse atrophy. This is a common cause in conditions where individuals are unable to move or exercise normally.
Aging (Sarcopenia): Aging leads to a natural decline in muscle mass and strength, a process known as sarcopenia. This occurs due to hormonal changes, reduced physical activity, and alterations in protein metabolism.
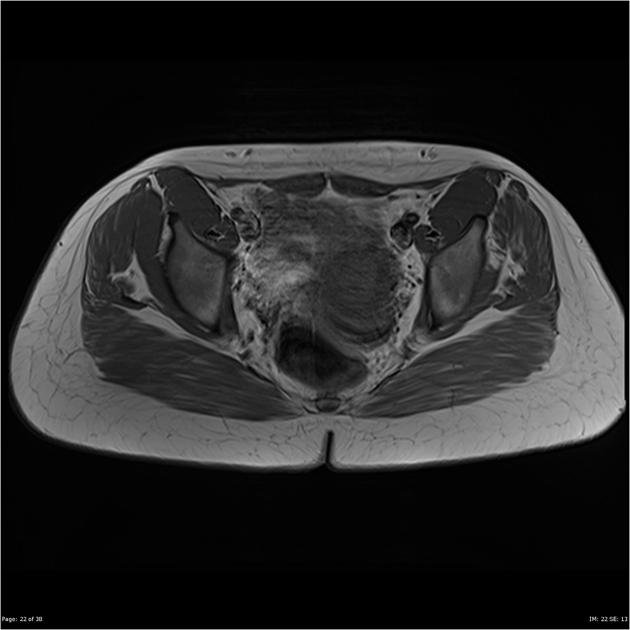
Neurological Conditions: Disorders affecting the nerves that control muscles, such as spinal cord injuries, stroke, neuropathies, and motor neuron diseases (like ALS), can lead to muscle weakness and atrophy.
Chronic Illnesses: Chronic diseases such as cancer, heart failure, chronic obstructive pulmonary disease (COPD), and kidney disease can cause muscle wasting. These conditions often involve inflammation, hormonal imbalances, and metabolic changes that contribute to muscle protein breakdown.
Malnutrition and Cachexia: Inadequate nutrition, especially protein deficiency, can impair muscle protein synthesis and lead to muscle atrophy. Cachexia, a severe form of malnutrition often associated with advanced cancer and other chronic diseases, involves significant muscle wasting.
Endocrine Disorders: Hormonal imbalances, such as low testosterone levels (hypogonadism) or excess cortisol (Cushing’s syndrome), can contribute to muscle loss.
Medications: Certain medications, such as corticosteroids (used to treat inflammation and autoimmune conditions), can cause muscle weakness and atrophy as a side effect.
Genetic Factors: Inherited conditions that affect muscle structure or function can lead to progressive muscle wasting, such as muscular dystrophies.
Severe Trauma or Burns: Major trauma, severe burns, or surgical procedures that require prolonged immobilization can result in muscle atrophy due to reduced physical activity and tissue damage.
Spaceflight: Astronauts experience muscle atrophy due to the microgravity environment of space, which reduces the mechanical loading on muscles and leads to rapid muscle loss
Treatment
Physical Therapy and Exercise:
- Resistance Training: Strength training exercises that target specific muscle groups can help stimulate muscle growth and prevent further muscle loss.
- Range of Motion Exercises: These exercises maintain joint flexibility and prevent stiffness, especially important during periods of immobilization.
- Functional Training: Activities that mimic daily movements can improve overall muscle function and coordination.
Nutritional Support:
- Protein Intake: Adequate protein consumption is essential for muscle maintenance and repair. Protein-rich foods and supplements may be recommended, especially in cases of malnutrition or cachexia.
- Caloric Intake: Ensuring sufficient calories to meet energy needs and support muscle recovery is crucial.
- Micronutrients: Certain vitamins and minerals, such as vitamin D and calcium, play roles in muscle function and bone health.
Medical Treatments:
- Medications: In some cases, medications may be prescribed to address underlying conditions contributing to muscle atrophy, such as hormonal therapies or medications to manage inflammation.
- Anabolic Steroids: These medications may be used in specific clinical situations to promote muscle growth and counteract muscle loss.
Electrical Stimulation:
- Neuromuscular Electrical Stimulation (NMES): Electrical currents applied to muscles can help maintain muscle strength and prevent atrophy, particularly in individuals who are unable to perform conventional exercises.
Surgical Interventions:
- Surgery: In cases of severe muscle damage or loss due to trauma or certain conditions, surgical interventions such as tendon transfers or muscle grafts may be considered to restore function.
Management of Underlying Conditions:
- Physical Rehabilitation: Rehabilitative therapies tailored to the specific condition causing muscle atrophy, such as stroke rehabilitation or spinal cord injury rehabilitation.
- Disease-Specific Treatments: Treating and managing underlying diseases or conditions that contribute to muscle wasting, such as cancer, neurological disorders, or chronic inflammatory diseases.
Psychosocial Support:
- Counseling and Support Groups: Psychological support can help individuals cope with the emotional and social challenges of living with muscle atrophy and its impact on daily life.