Abdominal Aortic Aneurysm
content of this page
1- Introduction
2- Anatomical Overview
3- Treatment
4- purposes
Introduction
An Abdominal Aortic Aneurysm (AAA) is a localized enlargement of the abdominal aorta, the largest artery in the abdomen, which can lead to a life-threatening rupture if it grows too large. This condition typically occurs when the walls of the aorta weaken and begin to bulge. Risk factors include advanced age, smoking, high blood pressure, and a family history of aneurysms.
Anatomical Overview
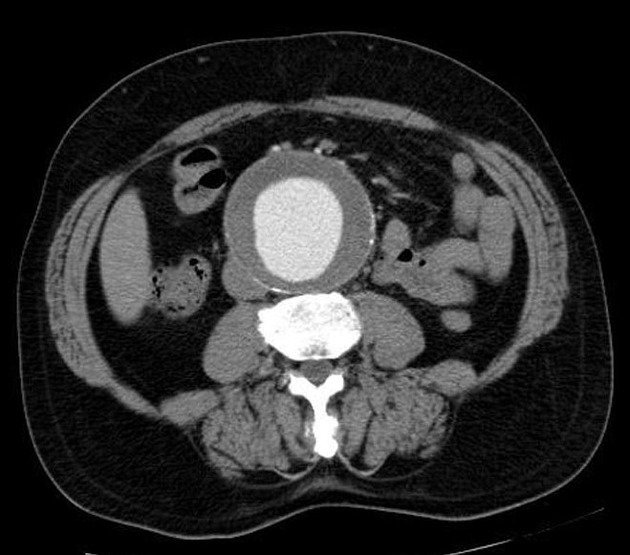
The abdominal aorta begins just below the diaphragm and extends to the level of the fourth lumbar vertebra, where it bifurcates into the right and left common iliac arteries. An AAA involves a balloon-like dilation of the aortic wall, typically defined as a dilation greater than 3 cm, compared to the normal diameter of about 2 cm. This bulging results from a weakening of the aortic wall, often due to factors like atherosclerosis, hypertension, and genetic predispositions.
The aorta has three layers: the intima (inner layer), media (middle layer), and adventitia (outer layer). An aneurysm usually involves the weakening and bulging of these layers. The abdominal aorta runs anteriorly to the spine, with the renal arteries branching off to supply the kidneys and the inferior vena cava running parallel to return deoxygenated blood from the lower body to the heart. An AAA can sometimes exert pressure on the spine and surrounding nerves, causing back pain.
The primary concern with an AAA is the risk of rupture, which can lead to life-threatening internal bleeding. Many AAAs are asymptomatic, but symptoms, when present, may include abdominal pain, back pain, and a pulsating sensation in the abdomen. AAAs are often discovered incidentally through imaging studies like ultrasound, CT scans, or MRI. Regular monitoring is essential to track the size and growth rate of the aneurysm

Treatment
Watchful Waiting:
- Monitoring: For small AAAs (less than 5.5 cm in diameter), regular monitoring through ultrasound or CT scans is often recommended. The frequency of monitoring depends on the size and growth rate of the aneurysm.
- Lifestyle Modifications: Patients are advised to quit smoking, manage blood pressure, and adopt a healthy diet and exercise regimen to slow the growth of the aneurysm.
Medical Management:
- Medications: Antihypertensive drugs (like beta-blockers) may be prescribed to control blood pressure and reduce stress on the aortic wall. Statins may also be used to manage cholesterol levels and reduce atherosclerosis.
Surgical Intervention:
- Open Repair: This traditional method involves a large abdominal incision to directly access the aorta. The surgeon replaces the weakened section of the aorta with a synthetic graft. This approach is effective but has a longer recovery time and higher risk compared to less invasive methods.
- Endovascular Aneurysm Repair (EVAR): A less invasive procedure, EVAR involves inserting a catheter through the femoral artery in the groin to place a stent-graft inside the aneurysm. This graft reinforces the weakened area and creates a new path for blood flow, reducing pressure on the aneurysm. EVAR typically has a shorter recovery time and fewer immediate risks compared to open repair.
Purposes
- Prevent Rupture: The main goal is to reduce the risk of the aneurysm rupturing.
- Manage Symptoms: For symptomatic aneurysms, treatment aims to alleviate pain and discomfort.
- Improve Survival: Effective treatment reduces mortality associated with ruptured AAAs.
- Enhance Quality of Life: Minimizing the risk of rupture and managing symptoms contribute to better overall quality of life.