Jugular Venous Pulse
content of this page
1- Introduction
2- Anatomical Overview
3- Procedure
4- Clinical Significance
Introduction
The Jugular Venous Pulse (JVP) is a critical physiological indicator that provides valuable insights into the function of the heart and the volume status of a patient. Located in the right internal jugular vein, the JVP reflects the pressure dynamics within the right atrium of the heart. This pulsation is observable in the neck and varies with cardiac cycles, offering clinicians a non-invasive means to assess cardiovascular health.
Anatomical Overview
Internal Jugular Vein (IJV):
- The internal jugular vein is one of the principal veins draining blood from the brain, face, and neck.
- It runs alongside the common carotid artery in the neck, usually within the carotid sheath, which also contains the vagus nerve and the carotid artery.
- The right internal jugular vein is preferred for assessing the JVP due to its direct path to the right atrium of the heart.
Right Atrium:
- The right internal jugular vein terminates in the right atrium of the heart.
- It is here that the venous blood from the upper body collects before being pumped into the right ventricle and then to the lungs for oxygenation.
Valves and Waves:
- The JVP exhibits specific waves and contours that correspond to different phases of the cardiac cycle:
- a wave: Produced by atrial contraction.
- c wave: Caused by the bulging of the tricuspid valve into the right atrium during ventricular contraction.
- v wave: Due to atrial filling against a closed tricuspid valve during ventricular systole.
- The JVP exhibits specific waves and contours that correspond to different phases of the cardiac cycle:
Anatomical Landmarks:
- Clinicians use specific anatomical landmarks on the neck to assess the JVP, such as the sternal angle (Angle of Louis) and the right atrium.
- The sternal angle corresponds approximately to the level of the right atrium and is often used as a reference point to measure the height of the JVP.
Clinical Significance:
- The JVP is a valuable indicator of cardiovascular health and volume status.
- Changes in JVP height, waveform, and response to maneuvers like the hepatojugular reflux can provide diagnostic clues for conditions such as heart failure, fluid overload, or constrictive pericarditis.

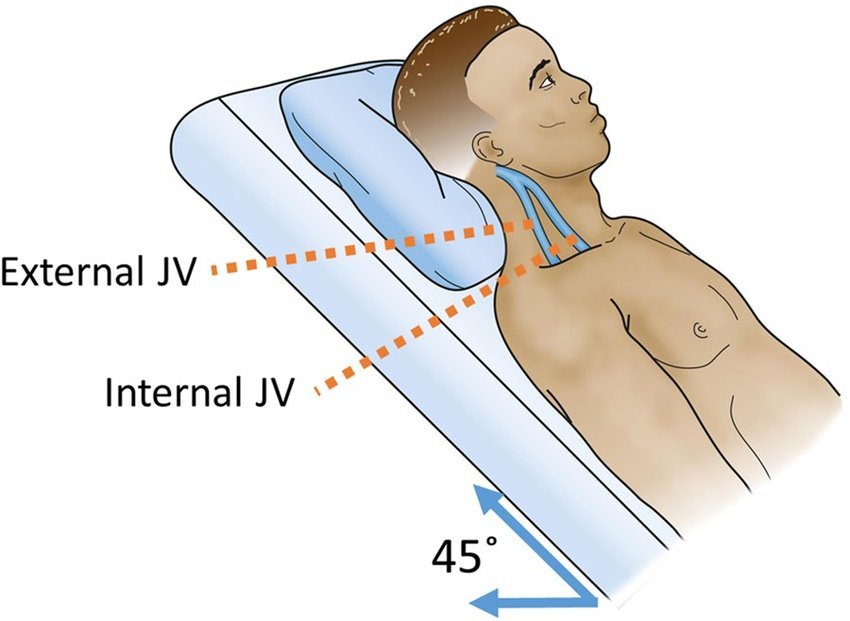
Procedure
Although pulsations are most commonly associated with arteries, pulsations of the (IJV) can provide information about heart activity corresponding to electrocardiogram (ECG) recordings and right atrial pressure. The IJV pulse is not palpable in the same manner as arterial pulses; however, the vein’s pulsations are transmitted through the surrounding tissue and may be observed beneath the SCM superior to the medial end of the clavicle. Because there are no valves in the brachiocephalic vein or the superior vena cava, a wave of contraction passes up these vessels to the inferior bulb of the IJV. The pulsations are especially visible when the person’s head is inferior to the lower limbs (Trendelenburg position). The internal jugular pulse increases considerably in conditions such as mitral valve disease, which increases pressure in the pulmonary circulation and right side of the heart. The right IJV runs a straighter, more direct course to the right atrium than does the left; therefore, it is the one that is examined (Bickley, 2016).
Clinical Significance
Assessment of Fluid Status:
- The JVP is a reliable indicator of fluid status, particularly volume overload (hypervolemia) or depletion (hypovolemia). An elevated JVP often indicates increased venous pressure due to fluid overload, as seen in conditions like congestive heart failure or renal failure. Conversely, a low or flat JVP may suggest hypovolemia, dehydration, or blood loss.
Diagnosis of Cardiac Conditions:
- Changes in the JVP waveform and contour can provide diagnostic clues for various cardiac conditions:
- Heart Failure: Elevated JVP with prominent v waves may indicate right-sided heart failure, whereas a prominent a wave can suggest left-sided heart failure.
- Constrictive Pericarditis: Characteristic “Kussmaul’s sign” may be observed—a paradoxical increase in JVP during inspiration due to impaired right ventricular filling.
- Cardiac Tamponade: Elevated JVP with a prominent x descent and absent y descent due to impaired filling of the right ventricle in diastole.
- Changes in the JVP waveform and contour can provide diagnostic clues for various cardiac conditions:
Monitoring Response to Therapy:
- Serial assessment of JVP helps monitor the response to treatment in heart failure and other cardiovascular conditions. A decrease in JVP height and normalization of waveform may indicate effective management of fluid status and improvement in cardiac function.
Guiding Fluid Management:
- In critically ill patients, monitoring the JVP assists in guiding fluid resuscitation. It helps clinicians optimize fluid balance, avoid fluid overload complications (e.g., pulmonary edema), and maintain adequate tissue perfusion.
Differentiation of Dyspnea Causes:
- JVP assessment aids in distinguishing between cardiac and non-cardiac causes of dyspnea. Elevated JVP supports the diagnosis of heart failure, while normal JVP suggests other etiologies such as chronic obstructive pulmonary disease (COPD) exacerbation or pulmonary embolism.
Assessment of Right Atrial Pressure:
- The JVP provides an indirect measure of right atrial pressure. Clinicians use this information to estimate central venous pressure, which guides therapeutic decisions such as the initiation or adjustment of diuretic therapy.
Evaluation of Venous Return and Cardiac Output:
- The JVP reflects the dynamics of venous return to the heart and influences cardiac output. Changes in JVP characteristics can indicate alterations in venous return and potentially impact cardiac output and tissue perfusion.