Bone Grafting
content of this page
1- Introduction
2- Anatomical Overview
3- Procedure
4- Clinical Significance
Introduction
Bone grafting of the lower limb is a specialized surgical procedure aimed at addressing a wide range of conditions affecting the bones of the legs and feet. Whether due to trauma, infection, tumors, or congenital deformities, situations may arise where bone tissue needs repair, replacement, or augmentation to restore function and structural integrity. This intricate procedure involves transplanting bone from either the patient’s own body (autograft) or a donor (allograft) to the affected area. By promoting healing, supporting bone growth, and stabilizing fractures or defects, bone grafting of the lower limb plays a pivotal role in enabling patients to regain mobility, alleviate pain, and achieve better overall quality of life. This introduction sets the stage for exploring the various applications, techniques, and benefits associated with bone grafting in lower limb orthopedic surgery.
Anatomical Overview
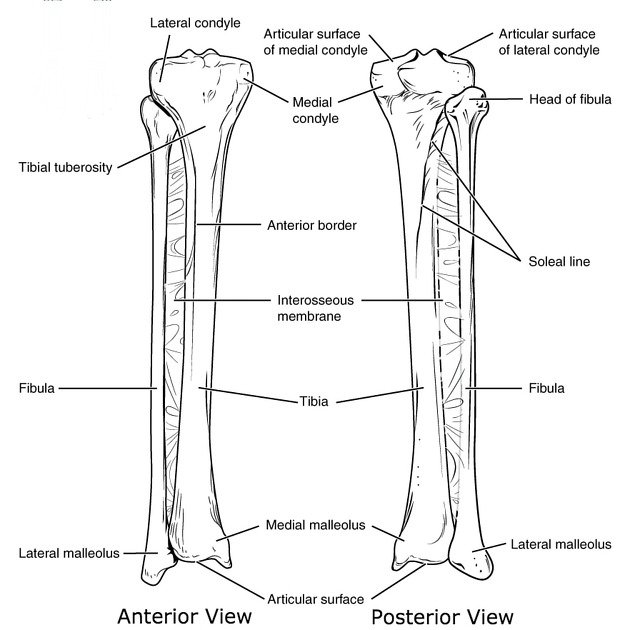
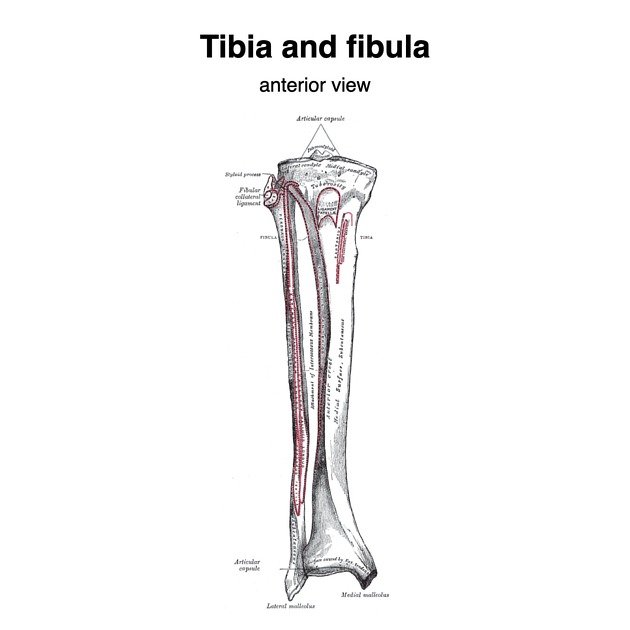
Bone grafting of the lower limb involves intricate knowledge of the anatomy and function of the bones, joints, and surrounding tissues. Here’s an anatomical overview:
Bones of the Lower Limb: The lower limb includes the femur (thigh bone), patella (kneecap), tibia and fibula (lower leg bones), and the bones of the foot (metatarsals, tarsals, phalanges). Each bone has specific roles in weight-bearing, movement, and stability.
Joints: Joints such as the hip, knee, ankle, and various smaller joints of the foot facilitate movement and weight distribution. These joints are critical for mobility and stability.
Muscles and Tendons: Muscles of the lower limb, including the quadriceps, hamstrings, calf muscles, and intrinsic foot muscles, provide strength and support. Tendons connect muscles to bones, allowing for movement and stability.
Blood Supply: The lower limb has an extensive network of blood vessels (arteries and veins) that supply oxygen and nutrients to bones and tissues, crucial for healing and recovery post-surgery.
Nerves: Nerves of the lower limb, including the sciatic nerve and branches such as the femoral nerve, provide sensation and control muscle movement. Preservation of nerve function is essential during surgery to maintain proper limb function.
Soft Tissues: Ligaments, cartilage, and fascia provide structural support and help maintain joint stability. These tissues are important considerations during bone grafting to ensure proper alignment and function.
Bone Marrow: Bone marrow within the bones of the lower limb is responsible for producing blood cells and contains stem cells crucial for bone regeneration and healing.
Procedure
Preoperative Preparation:
Patient Evaluation: The patient undergoes a thorough evaluation, including medical history, physical examination, and imaging studies (X-rays, CT scans, MRI) to assess the extent of bone damage or defects.
Surgical Planning: Based on the evaluation, the surgeon determines the type of bone graft (autograft, allograft, synthetic graft), the size and shape of the graft needed, and the surgical approach.
Surgical Procedure:
Anesthesia: The patient is placed under general anesthesia or regional anesthesia (spinal or epidural) to ensure comfort and pain control during the procedure.
Incision: The surgeon makes an incision over the affected area of the lower limb to access the bone defect. The location and size of the incision depend on the specific condition being treated.
Preparation of Recipient Site: The surgeon carefully prepares the recipient site by removing damaged or non-viable bone tissue, ensuring a healthy bed for the graft.
Harvesting the Graft: Depending on the chosen graft type:
- Autograft: Bone tissue is harvested from another part of the patient’s body (commonly the iliac crest of the hip, fibula, or proximal tibia).
- Allograft: Donor bone tissue sourced from a bone bank is prepared and shaped to fit the defect.
- Synthetic Graft: Artificial materials designed to mimic bone structure may be used in some cases.
Graft Placement: The harvested or prepared bone graft is meticulously placed into the defect site. The surgeon ensures proper alignment and fit to promote healing and integration with surrounding bone tissue.
Fixation: In some cases, fixation devices such as screws, plates, or rods may be used to secure the graft in place and provide stability during the healing process.
Closure: The incision is closed with sutures or staples. Drains may be placed to remove excess fluid from the surgical site.
Postoperative Care:
Recovery: The patient is monitored closely in the recovery room and then in the hospital ward. Pain management and antibiotic therapy may be administered as needed.
Physical Therapy: Rehabilitation begins early to promote mobility, strengthen muscles, and prevent stiffness. Range of motion exercises and weight-bearing activities are gradually introduced based on healing progress.
Follow-up: Regular follow-up visits with the surgeon are scheduled to monitor healing, assess graft integration, and manage any complications that may arise.
Risks and Complications:
- Infection: Risk of infection at the surgical site.
- Graft Failure: Poor integration of the graft with existing bone.
- Nerve or Blood Vessel Injury: Damage to nearby structures during surgery.
- Delayed Healing: Prolonged recovery time or non-union of bones.
Clinical Significance
Fracture Repair: Bone grafting is crucial in cases where fractures of the lower limb have difficulty healing (non-union) or where there is significant bone loss. The graft provides structural support and promotes bone union by enhancing the body’s natural healing process.
Bone Defects: Conditions such as bone tumors, infections (osteomyelitis), or congenital deformities can result in large bone defects. Bone grafting helps to fill these defects, restore bone integrity, and prevent complications such as instability or limb length discrepancies.
Joint Reconstruction: In cases of severe joint damage or degeneration (e.g., advanced osteoarthritis), bone grafting may be used as part of joint reconstruction procedures. It helps to rebuild bone structures and support prosthetic implants, improving joint function and reducing pain.
Orthopedic Surgeries: Bone grafting is integral in various orthopedic surgeries of the lower limb, including joint replacements, corrective osteotomies (bone reshaping), and limb lengthening procedures. It ensures adequate bone support and stability for successful surgical outcomes.
Maxillofacial Reconstruction: In complex cases involving facial trauma or congenital anomalies affecting the lower jaw or facial bones, bone grafting techniques may extend to the lower facial and mandibular regions to restore form and function.
Enhancing Bone Healing: In elective orthopedic procedures, such as spine fusions or bone grafts for stress fractures, bone grafting accelerates healing and improves the likelihood of achieving solid bone union.
Dental Implantology: Bone grafting is also utilized in dental implantology, particularly in the lower jaw, to augment bone volume for successful implant placement and stability.
Biological Repair: Beyond structural support, bone grafting provides a biological scaffold that promotes the recruitment of osteogenic cells, growth factors, and cytokines necessary for new bone formation and remodeling.